|
 |
- Search
Article category
- Page Path
-
- HOME
- ARTICLE CATEGORY
- Article category
- IBD
- Effect of resistance exercise training on Crohn’s disease patients
- Konstantinos Papadimitriou
- Intest Res. 2021;19(3):275-281. Published online November 20, 2020
- Full text PubReader ePub PDF

- Management of Clostridioides difficile infection in patients with inflammatory bowel disease
- Sahil Khanna
- Intest Res. 2021;19(3):265-274. Published online August 18, 2020
- Full text PubReader ePub PDF

 |
 |
- Correlation of serum levels of anti-tumor necrosis factor agents with perianal fistula healing in Crohn’s disease: a narrative review
- Eron Fabio Miranda, Rodrigo Bremer Nones, Paulo Gustavo Kotze
- Intest Res. 2021;19(3):255-264. Published online November 6, 2020
- Full text PubReader ePub PDF

 |
 |
- Miscellaneous
- Bloating in a supine position
- Akira Hokama, Yasuka Nakada, Aki Yanagida, Erika Koga, Kunikazu Hoshino, Jiro Fujita
- Intest Res. 2021;19(2):252-253. Published online June 18, 2020
- Full text PubReader ePub PDF

 |
 |
- IBD
- Non-cirrhotic portal hypertension related to azathioprine therapy in a patient with Crohn’s disease
- Jong Won Seo, Eun Soo Kim, Man-Hoon Han, Young Oh Kweon
- Intest Res. 2021;19(2):247-251. Published online July 2, 2020
- Full text PubReader ePub PDF

 |
 |
- Colorectal Tumors
- Postgastrectomy gastric cancer patients are at high risk for colorectal neoplasia: a case control study
- Tae-Geun Gweon, Kyu-Tae Yoon, Chang Hyun Kim, Jin-Jo Kim
- Intest Res. 2021;19(2):239-246. Published online November 13, 2020
- Full text PubReader ePub PDF

 |
 |
- Inflammatory Bowel Diseases
- Prospective validation of CD4+CD25+FOXP3+ T-regulatory cells as an immunological marker to differentiate intestinal tuberculosis from Crohn’s disease
- Ritika Rampal, Saurabh Kedia, Mohamad Nahidul Wari, Deepak Madhu, Amit Kumar Singh, Veena Tiwari, V. Pratap Mouli, Srikant Mohta, Govind Makharia, Vineet Ahuja
- Intest Res. 2021;19(2):232-238. Published online May 8, 2020
- Full text PubReader ePub PDF

 |
 |
- Effect of acid-reducing agents on clinical relapse in ulcerative colitis with pH-dependent-released 5-aminosalicylic acid: a multicenter retrospective study in Japan
- Yosuke Shimodaira, Kengo Onochi, Kenta Watanabe, So Takahashi, Sho Fukuda, Noboru Watanabe, Shigeto Koizumi, Tamotsu Matsuhashi, Katsunori Iijima
- Intest Res. 2021;19(2):225-231. Published online August 18, 2020
- Full text PubReader ePub PDF

 |
 |
- Ustekinumab for the treatment of refractory pediatric Crohn’s disease: a single-center experience
- Alexandra Cohen, Najma Ahmed, Ana Sant’Anna
- Intest Res. 2021;19(2):217-224. Published online April 22, 2020
- Full text PubReader ePub PDF

 |
 |
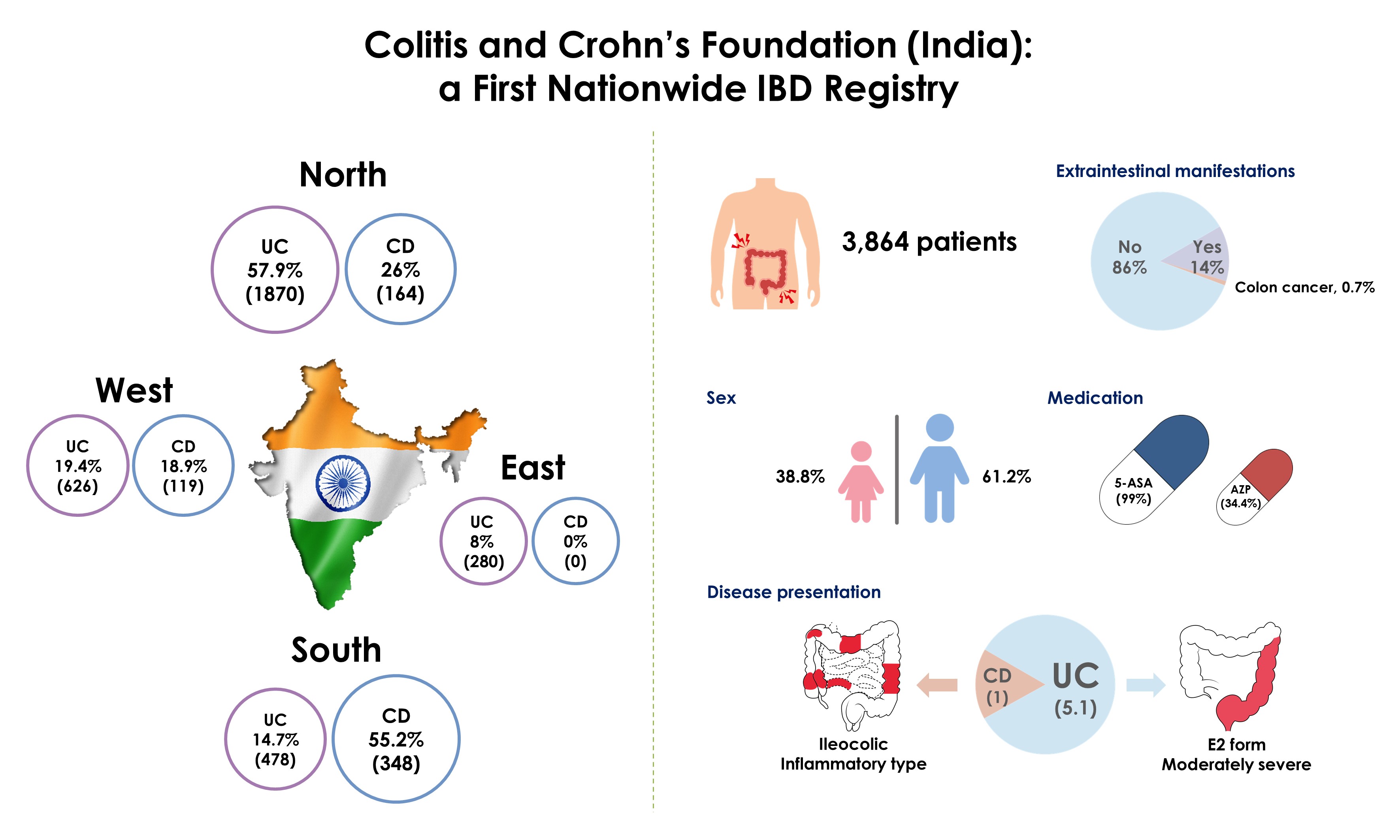
- Colitis and Crohn’s Foundation (India): a first nationwide inflammatory bowel disease registry
- Ajit Sood, Kirandeep Kaur, Ramit Mahajan, Vandana Midha, Arshdeep Singh, Sarit Sharma, Amarender Singh Puri, Bhabhadev Goswami, Devendra Desai, C. Ganesh Pai, Kiran Peddi, Mathew Philip, Rakesh Kochhar, Sandeep Nijhawan, Shobna Bhatia, N. Sridhara Rao
- Intest Res. 2021;19(2):206-216. Published online July 13, 2020
- Full text PubReader ePub PDF

 |
 |
- Yarrow oil ameliorates ulcerative colitis in mice model via regulating the NF-κB and PPAR-γ pathways
- Maged E. Mohamed, Sahar A. Elsayed, Hafez R. Madkor, Heba M. Saad Eldien, Omar M. Mohafez
- Intest Res. 2021;19(2):194-205. Published online August 21, 2020
- Full text PubReader ePub PDF

 |
 |
- Temporal trend in the natural history of ulcerative colitis in a country with a low incidence of ulcerative colitis from 2000 through 2018
- Satimai Aniwan, Julajak Limsrivilai, Supot Pongprasobchai, Nonthalee Pausawasdi, Piyapan Prueksapanich, Natanong Kongtub, Rungsun Rerknimitr
- Intest Res. 2021;19(2):186-193. Published online August 18, 2020
- Full text PubReader ePub PDF

 |
 |
- IBD
- Anti-inflammatory diet and inflammatory bowel disease: what clinicians and patients should know?
- Nor Hamizah Shafiee, Zahara Abdul Manaf, Norfilza M. Mokhtar, Raja Affendi Raja Ali
- Intest Res. 2021;19(2):171-185. Published online February 3, 2021
- Full text PubReader ePub PDF

 |
 |
- The impact of tobacco smoking on treatment choice and efficacy in inflammatory bowel disease
- Steven Nicolaides, Abhinav Vasudevan, Tony Long, Daniel van Langenberg
- Intest Res. 2021;19(2):158-170. Published online October 13, 2020
- Full text PubReader ePub PDF

 |
 |
- Cancer
- Clinical practice guideline for endoscopic resection of early gastrointestinal cancer
- Chan Hyuk Park, Dong-Hoon Yang, Jong Wook Kim, Jie-Hyun Kim, Ji Hyun Kim, Yang Won Min, Si Hyung Lee, Jung Ho Bae, Hyunsoo Chung, Kee Don Choi, Jun Chul Park, Hyuk Lee, Min-Seob Kwak, Bun Kim, Hyun Jung Lee, Hye Seung Lee, Miyoung Choi, Dong-Ah Park, Jong Yeul Lee, Jeong-Sik Byeon, Chan Guk Park, Joo Young Cho, Soo Teik Lee, Hoon Jai Chun
- Intest Res. 2021;19(2):127-157. Published online October 13, 2020
- Full text PubReader ePub PDF Supplementary Material

 |
 |