The evolving understanding of histology as an endpoint in ulcerative colitis
Article information
Abstract
A therapeutic goal for patients with ulcerative colitis (UC) is deep remission including clinical remission and mucosal healing. Mucosal healing was previously defined by endoscopic appearance, but recent studies demonstrate that histological improvements can minimize the risks of experiencing clinical relapse after achieving endoscopic remission, and there is growing interest in the value and feasibility of histological targets of treatment in inflammatory bowel disease, and specifically UC. In this review article, we identify remaining challenges and discuss an evolving role of histology in the management of UC.
INTRODUCTION
Deep remission is the current therapeutic goal for patients with ulcerative colitis (UC). The most common components of deep remission are clinical remission and mucosal healing. Previously, the majority of clinical trials for patients with UC defined mucosal healing as a Mayo endoscopic subscore [1] of 0 or 1. This level of mucosal healing was associated with long-term clinical remission, avoidance of colectomy, and corticosteroid-free clinical remission in patients with UC [2].
The definition of mucosal healing has evolved to include not only endoscopic improvement, but also to include assessments of histological healing. Even in patients with UC achieving endoscopic remission, histologically active inflammation can be observed [3,4] and histological remission appears to be associated with improved clinical outcomes [5]. Although the classification of histological inflammation varies among studies, the Geboes score (GS) [6], the Robarts histopathology index (RHI) [7], and the Nancy index (NI) [8] are considered appropriate for assessing histological activity in patients with UC [9]. However, these scoring systems do not include a category of “normal” histology, despite recent evidence demonstrating the possibility and clinical value of histological normalization in all of colonic segments in reducing the risks of clinical recurrence [10] and associated with a lower risk of colorectal neoplasia in patients with UC [11].
In this review, we discuss the therapeutic targets, the role of histological normalization on clinical outcomes, and histological inflammation classifications for patients with UC.
THERAPEUTIC TARGETS FOR PATIENTS WITH UC
Current management strategies for patients with UC advocate deep remission, including clinical remission and normalization of objective measures of disease control as the therapeutic goal. The Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE-I) consensus statement previously proposed that the agreed targets for UC were composite endpoints including endoscopic remission and clinical/patient-reported outcome remission [12]. The recommendations are based on the evidence supporting that the degree of “mucosal healing” is associated with clinical outcomes including colectomy [13]. In the clinical trials of biologics or small-molecule agents for patients with UC, mucosal healing was often defined as Mayo endoscopic subscore [1] 0 or 1 [14-18]. A meta-analysis demonstrated that mucosal healing was associated with long-term clinical remission, avoidance of colectomy, and corticosteroid-free clinical remission [2].
Numerous studies have contributed to our current understanding of histological remission’s impact on clinical outcomes in patients with UC. In the 1990s, several studies found that histologically active inflammation could be observed even if patients achieved endoscopic remission and it was predictive of clinical relapse [3,4]. In the 2000s, many studies underscored the correlation between residual histological activity and adverse clinical outcomes in patients with UC, although histological measurements varied among studies [19]. A meta-analysis including 10 studies of 757 patients in endoscopic remission (Mayo endoscopic subscore 0) showed a 63% lower risk of clinical relapse in patients with histological remission compared with those with persistent histological activity. This study also found only a 5% estimated annual risk of clinical relapse in patients who achieved both of histological remission and Mayo endoscopic subscore 0 [5]. Another meta-analysis including 2,677 patients with UC demonstrated that histologically active disease was associated with an overall increased risk of relapse (odds ratio, 2.4; 95% confidence interval [CI], 1.9–3.0), with a similar trend noted in either patients with Mayo endoscopic subscore 0 or those with subscore 0 or 1 [20]. A recent meta-analysis compared short- and long-term clinical outcomes between patients with inflammatory bowel disease (IBD) who achieved histological remission and those with active histological disease. This study revealed that the risk of clinical relapse was significantly higher in patients with active histological disease in both short-term and long-term outcome analyses. In addition, the long-term outcome analysis showed that the risk of needing surgery and hospitalization was significantly higher in patients with active histological disease [21]. These meta-analyses suggest that using histological inflammation as a therapeutic target may improve clinical outcomes even if patients with UC achieved endoscopic remission.
Furthermore, several studies showed that histological inflammation increased the risk of colorectal neoplasia [22-24]. A group at St. Mark’s Hospital reported a novel cumulative inflammatory burden defined as the summation of each procedure’s microscopic inflammation severity score multiplied by the length of the surveillance interval [25]. They demonstrated that both endoscopic and histological cumulative inflammatory burdens were significantly associated with the risk of colorectal neoplasia [25]. This result was validated with an independent, matched case-controlled cohort from our IBD center [26]. Our recent study also revealed that histological normalization was associated with a decreased risk of subsequent dysplasia development in patients with UC [11].
Recently, the updated STRIDE statement (STRIDE-II) proposed that histological healing in UC is not yet a formal target but should be assessed to understand the depth of remission [27].
CLASSIFICATIONS OF HISTOLOGICAL INFLAMMATION IN PATIENTS WITH UC
The rate of histological remission for current medical treatments ranged from 15% to 45% in patients with UC [28]. To assess histological activity for UC, there are multiple scoring/grading systems, including the most commonly employed: the GS [6], RHI [7], and NI [8] (Fig. 1). The GS is the most commonly used histological score for patients with UC and had a structured 6-grade classification: (0) structural changes; (1) chronic inflammation; (2) lamina propria neutrophils; (3) neutrophils in the epithelium; (4) crypt destruction; and (5) erosions and ulcers [6]. Each of these grades has 4 to 5 sub-grades [6]. Currently, the GS has been used as a continuous scale and yield a final score between 0 and 22 (Fig. 1) [29,30].
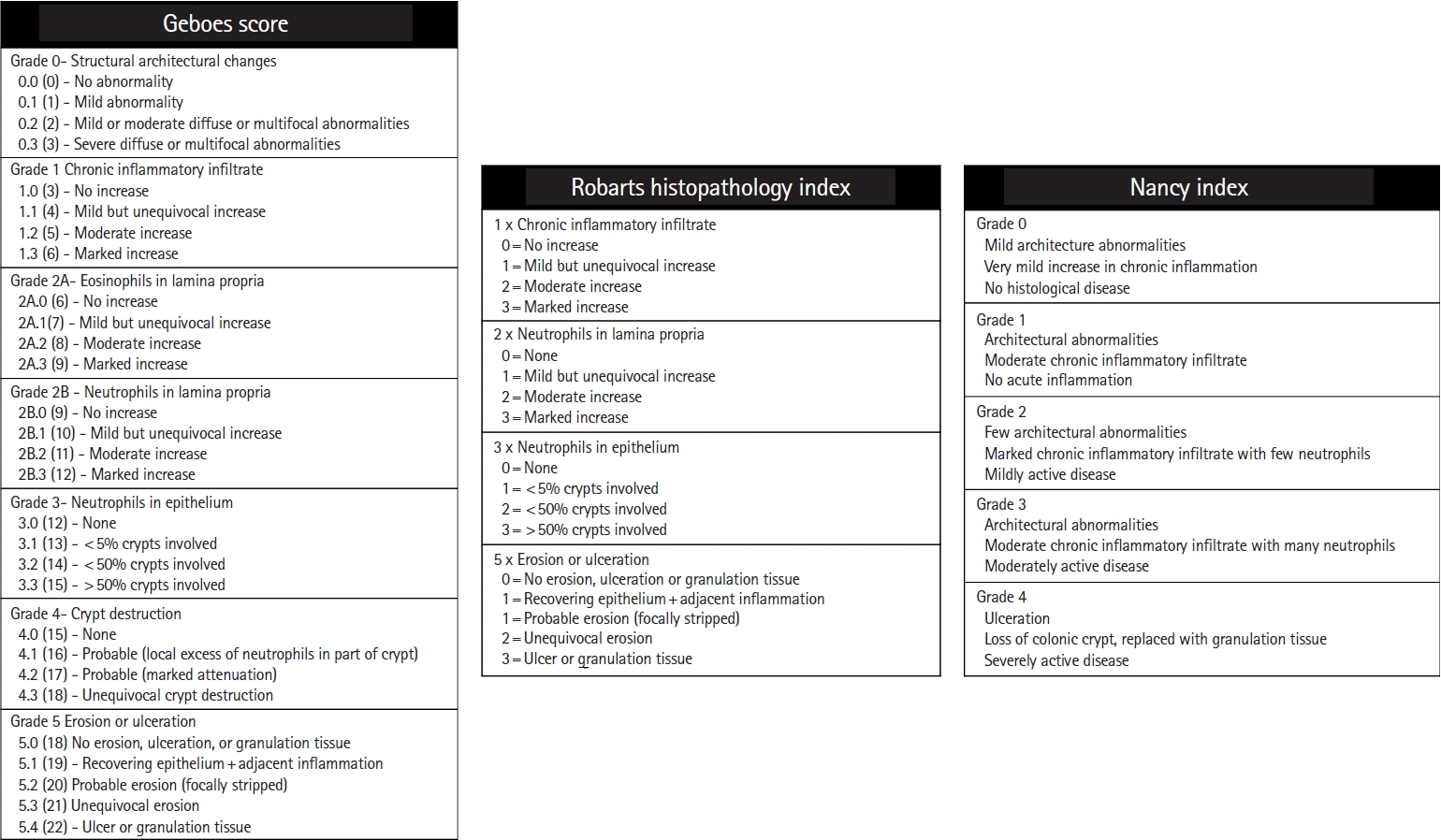
The classification of histologic inflammation for patients with ulcerative colitis. Tables showed Geboes score, Robarts histopathology index, and the Nancy index. In the table of Geboes score, numbers in parentheses show continuous score of Geboes score.
An RHI score is calculated by combining the subscore of the following 4 main items: (1) chronic inflammatory infiltrate; (2) neutrophils in the lamina propria; (3) neutrophils in the epithelium; and (4) erosion or ulceration [7]. As for the NI, ulceration, acute, and chronic inflammatory infiltrates are taken into account to calculate the score [8]. The Portuguese IBD Study Group showed that GS and RHI were strongly correlated (correlation coefficient 0.81) [30] and the correlation between GS and NI was also shown to be strongly correlated (correlation coefficient 0.88) [31]. They also demonstrated that the GS, RHI, and NI are well correlated with histological remission and activity and can be predictive of the Mayo endoscopic subscore [32]. This study found that higher fecal calprotectin levels were significantly associated with the presence of neutrophils in the epithelium [32]. Another prospective study showed that among the 3 histological indices, the RHI had the best correlation with the Mayo endoscopic subscore [33]. An international consensus to standardize integration of histopathology in UC clinical trials stated that the GS, RHI, and NI are each considered appropriate for assessing histological activity [9].
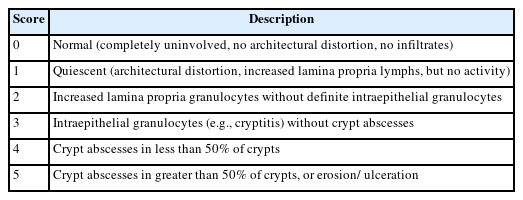
The common perception that structural histological changes are permanent upon IBD diagnosis has led to the exclusion of “normal” histology as a distinct category in these scoring systems. Our group previously established the University of Chicago scale to categorize the histological activity in patients with UC. In our classification, patients are categorized as (1) histologic normalization (score 0): completely normal mucosa with no features of chronicity present; (2) histologic quiescence (score 1): features of chronicity including crypt atrophy or branching but no active inflammation such as erosions, crypt abscesses, or focal neutrophils infiltration; and (3) histologic activity (score 2–5): presence of any epithelial infiltration by neutrophils, crypt abscesses, erosions or ulcerations (Table 1) [10,23]. Our studies found that 10% of patients achieved histologic normalization in all colonic segments (complete histologic normalization) and it was independently associated with increased odds of relapse-free survival compared with histologic quiescence (hazard ratio, 4.3; 95% CI, 1.5–12.5) and histologic activity (hazard ratio, 6.7; 95% CI, 2.2–20.6) [10].
COMPLETE HISTOLOGICAL NORMALIZATION VERSUS SEGMENTAL HISTOLOGICAL NORMALIZATION
The UNIFI study [18], a randomized controlled trial (RCT) of ustekinumab for patients with UC, included a combined histological and endoscopic improvement endpoint (histo-endoscopic mucosal healing) and demonstrated that histo-endoscopic mucosal healing is associated with lower disease activity compared with endpoints limited to histologic or endoscopic improvement alone.34 In this study, the rectum and sigmoid colon were selected to assess histological activity using the GS because they are typically the most severely inflamed parts in patients with UC [34]. A post hoc analysis of 3 clinical trials (PURSUIT-UC [35], JAK-UC [36], PROgECT [37]) also showed that histological improvement based on the GS was associated with favorable endoscopic and clinical outcomes in patients with UC. In this analysis, sample regions were to be 15–20 cm proximal to the anal verge and identical biopsy collections were used to evaluate histological improvement [38]. The U-ACHIEVE and U-ACCOMPLISH studies, RCTs to assess efficacy and safety of upadacitinib for patients with UC, defined mucosal healing as a combination of Mayo endoscopic subscore 0 and a GS < 2 [39]. In the studies, at least one set of biopsy are to be collected from the approximately 15 to 30 cm from the anal verge in the rectosigmoid colon with sigmoidoscopy or full colonoscopy, for each set of 2 samples, one should be taken from the most inflamed area, and the other from an area that is representative of the general severity of mucosal inflammation in the segment. Meanwhile, the True North study, an RCT of ozanimod for UC, used similar definition of mucosal healing (Mayo endoscopic subscore ≤ 1 and a GS < 2) and one biopsy pair was taken at the most inflamed area of the left colon with sigmoidoscopy or full colonoscopy [40]. Therefore, biopsy procedure varies among RCTs. A systematic review and meta-analysis including 13 randomized placebo-controlled trials demonstrated that histological outcomes may be informative for the assessment of disease activity in clinical trials for UC [41]. However, this study suggested that the lack of information regarding biopsy procedures is a limitation and there is a need to define standard biopsy procedures [41].
Recent studies suggest the importance of achieving histological remission in all colonic segments in patients with UC. Our group showed that segmental histological normalization occurs in 32% of patients with UC. Unlike complete histological normalization, segmental normalization was not associated with improved clinical outcomes [42]. Another study also demonstrated that the combination of pan-colonic endoscopic and histological evaluations may be beneficial to improve clinical outcomes in patients with UC [43].
Together, these findings suggest that to improve clinical outcomes in patients with UC, the rectum and sigmoid colon as well as the remaining segments of the colon should be taken into account while assessing histological activity.
OUTCOMES OF THERAPEUTIC DE-ESCALATION AFTER ACHIEVING REMISSION
Whether patients can withdraw medications after achieving remission remains an important question, and one that is incompletely explored involving histological measures. An expert consensus conducted by the European Crohn’s and Colitis Organisation (ECCO) stated the following considerations regarding withdrawal of each drug class in patients with IBD [44]. First, the withdrawal of anti-tumor necrosis factor (TNF) inhibitors is associated with a risk of relapse of 30% to 40% at 1 year and greater than 50% beyond 2 years, and patients who have needed anti-TNF dose escalation seem to be at higher risk. With such potential for risk of disease relapse in mind, anti-TNF withdrawal should probably be considered only in patients in “longstanding and stable deep remission” from a clinical, biological, and endoscopic standpoint [44]. Second, with regard to the de-escalation of immunomodulators, a cumulative risk of relapse after withdrawal of immunomodulators is estimated as about 30% of patients relapsing by 2 years and 50% to 75% relapsing by 5 years [44]. The consensus also stated that it is reasonable to reconsider the risks and benefits of continued monotherapy of immunomodulators for patients treated for 3 to 4 years if there is “no evidence of continuing disease activity.” It also suggested that the risk of relapse following withdrawal of immunomodulators is probably not greater than with continued combination therapy [44]. Given that long-term use of immunomodulators are considerably associated with risks of neoplasms such as lymphoproliferative disorders [45], non-melanoma skin cancers [46], and myeloid disorders [47], and combination with anti-TNF therapies may further potentiate risk of neoplasm and infection [44], periodic re-assessment of the risk and benefit of immunomodulator use would be important [44]. Third, on the other hand, the consensus by ECCO [44] recommended that aminosalicylates should not be discontinued even in patients with UC who achieve deep remission because long-term treatment of aminosalicylates is generally safe and reduces the risks of relapse [48] and colorectal cancer [49].
A systematic review and meta-analysis including 20 studies of IBD patients achieving clinical remission showed that clinical relapse rate was 0% to 54% when patients de-escalated the dose of biological therapies. This study also reported that 1-year rate of clinical relapse ranged from 7% to 50% [50], suggesting the high recurrence rates after de-escalation of biologics following clinical remission. Another meta-analysis including 5 studies of patients with UC with deep remission (at least combination of clinical remission and mucosal healing/endoscopic remission) reported that the rates of relapse within 1 year and 2 years of therapeutic de-escalation was 25.4% (95% CI, 19.9%–32.0%) and 37.4% (95% CI, 24.6%–52.4%), respectively. They also found that the risk of relapse was more pronounced in patients who required TNF inhibitors [51]. A recent multicenter open-label RCT of patients with UC who were in corticosteroid-free and endoscopic remission assessed the remission rate at week 48 between the infliximab-continued group and the infliximab-discontinued group. This study revealed that the remission rates in infliximab-continued group and discontinued group were 80% and 54%, respectively [52]. While studies assessing outcomes after discontinuation of non-TNF-targeted biologics remain scarce, a retrospective multicenter observational study evaluated maintenance of remission in patients with IBD after discontinuation of vedolizumab. This study included patients with IBD (37 with UC) who were in steroid-free clinical remission for at least 3 months and were treated with vedolizumab for at least 6 months and found that 64% of patients experienced disease relapse after a median follow-up period of 11.2 months [53]. As for Janus kinase (JAK) inhibitors, the pivotal RCTs conducted post hoc analyses of patients with UC who received drugs in induction and were randomized to treatment withdrawal (placebo) during maintenance, and demonstrated the efficacy and safety of re-treatment with JAK inhibitors in patients who experienced disease worsening [54,55]. However, it remains unclear how the depth of remission affects clinical outcomes after therapeutic withdrawal of JAK inhibitors in UC.
Previous studies suggest that deep remission may not endorse the success of therapeutic de-escalation in patients with UC. However, these studies do not necessarily include histological remission in their definition of deep remission. Several studies demonstrate that histological remission is a therapeutic target distinct from clinical remission [56] and endoscopic mucosal healing [57] in patients with UC. Hence, there is an unmet need to understand the clinical outcomes in UC patients who de-escalate therapies after achieving histological remission.
Furthermore, determining which classification of histological inflammation should be used is an important issue when considering therapeutic de-escalation or withdrawal. Although the GS, RHI, and NI would be appropriate in the clinical trials of patients with UC [9], these scoring systems do not have “normal” histology as a distinct category. Even in patients without active histological inflammation, features of chronicity such as crypt atrophy or branching can remain. Normalization of such histological structural abnormalities may improve clinical outcomes after therapeutic de-escalation or reduce the risk of colorectal neoplasia. Given that some studies suggest a positive association between pan-colonic histological normalization and favorable clinical outcomes in patients with UC [42,43], achieving normal histology in all colonic segments may be ideal.
REMAINING CHALLENGES TO THE INCORPORATION OF HISTOLOGICAL TARGETS IN UC
There are a number of significant challenges to incorporate histological activity as a treatment target in UC. First, there is a need for further studies demonstrating histological changes associated with medical therapies. Such studies must include information about the timing of histological improvement in relation to symptom improvement and in relation to endoscopic findings. Second, there is a need to standardize biopsy techniques, including number of biopsies, choice of location by segment and in relation to visible inflammation by endoscopic assessment. We have previously determined that a minimum number of biopsies can be obtained and are predictive of the histological activity of the rest of the colon and rectum [58]. Third, there is a need to standardize reporting and incorporation into clinical practice by pathologists. To date, the available scoring systems have not been incorporated into routine clinical reporting and inter-observer correlations amongst community pathologists have not been described. More recent efforts to incorporate artificial intelligence approaches using digital images suggest future approaches that might address this challenge (Table 2) [59].
CONCLUSIONS
While achieving normal histology in all segments of the colon in UC is ideal but not yet a formal goal, previous studies have shown that histological remission is associated with a decreased risk of clinical recurrence as well as the development of dysplasia. Overall, medical evidence regarding histology in patients with UC has evolved and so should our efforts to understand how histology can be used to develop better treatment plans for patients with UC.
Notes
Funding Source
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
Akiyama S reports no conflicts of interest. MIyatani Y has served as a speaker of AbbVie; received research funding from Japan Foundation for Applied Enzymology; and as an endowed chair of AbbVie, JIMRO, Zeria Pharmaceutical, Kyorin Pharmaceutical, Mochida Pharmaceutical, Otsuka Holdings, and EA Pharma. Rubin DT has received grant support from Takeda; and has served as a consultant for AbbVie, Abgenomics, Arena Pharmaceuticals, Bellatrix Pharmaceuticals, Boehringer Ingelheim Ltd., Bristol-Myers Squibb, Celgene, Syneos, Dizal Pharmaceuticals, Genentech/Roche, Gilead Sciences, Ichnos Sciences S.A., InDex Pharmaceuticals, Iterative Scopes, Janssen Pharmaceuticals, Lilly, Pfizer, Prometheus Laboratories, Reistone, Takeda, and Techlab Inc.
Rubin DT is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Data Availability Statement
Data is available upon reasonable request to the corresponding author.
Author Contributions
Conceptualization: Akiyama S, Rubin DT. Formal analysis; Investigation; Methodology; Project administration; Supervision: Rubin DT. Writing - original draft: Akiyama S, Rubin DT. Writing - review & editing: Akiyama S, Miyatani Y, Rubin DT. Approval of final manuscript: all authors.