A Case of Ascending Colonic Xanthoma Presenting as a Lateral Spreading Tumor
Article information
Abstract
Gastrointestinal xanthomas are characterized by foamy cytoplasmic cells containing lipid in lamina propria, and occur almost in the gastric mucosa. Colonic xanthomas have been described in rare case. All reported colonic xanthomas were located in rectosigmoid. Rectosigmoid xanthomas have tended to exhibit small polypoid lesion, on the contrary flat in stomach. We report a case of xanthoma on ascending colon presenting as a laterally spreading tumor resected by endoscopic mucosal resection method.
INTRODUCTION
Gastrointestinal xanthomas are characterized by cells with foamy cytoplasm containing lipid in lamina propria and commonly occur in the gastric mucosa.1 Colonic xanthomas have been rarely reported, and most colonic xanthoma cases have been found in the sigmoid colon and rectum.1 The authors experienced a rare case of ascending colonic xanthoma detected in a patient who underwent colonoscopy for health screening. We performed endoscopic mucosal resection (EMR) for the removal of laterally spreading tumor (LST) in the ascending colon and pathologically confirmed with xanthoma. Therefore, we report this case with a brief review of literature.
CASE REPORT
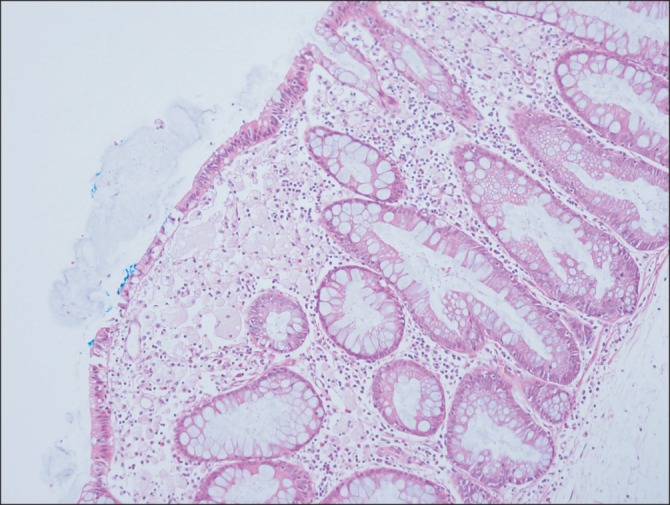
A 59-year old male patient visited our hospital to receive colonoscopy for a regular check-up. He had no specific findings in past medical and social history, and his blood pressure, temperature, and respiratory rate were all within normal range. Outpatient hematologic test revealed a white blood cell of 7,900/mm3, Hemoglobin of 14.3 g/dL, and platelet count of 236,000/mm3, and biochemical test revealed no abnormal findings. The patient was administered with a 4 L of colyte for 2 h as the pretreatment 6 h before performing colonoscopic exam, the bowel preparation was excellent when a colonoscope reached to the ceccum. A LST was a 15 mm flat elevated-type lesion focally associated with white spots in the ascending colon (Fig. 1). This lesion appeared flat in air filled distended bowel and folded in air sucked out colon. When the lesion was pushed by a biopsy forceps, the surface was pushed to the side. Saline was injected into the submucosal layer to lift the target lesion, and then EMR was performed to completely resected the swollen lesion using a snare (Fig. 2). There were no complications such as intra- or postoperative bleeding, perforation, and others. The lesion was diagnosed as xanthoma since biopsy revealed foam cells that contained neither mucin nor pigment in the submucosal layer (Fig. 3, 4). About a 4 mm sessile polyp was observed on the opposite site of xanthoma. The polyp was removed using biopsy forceps and biopsy diagnosed as tubular adenoma with low grade dysplasia.

Colonoscopic findings. The endoscopy showed about 15 mm sized laterally spreading tumor in the ascending colon.
DISCUSSION
Xanthoma is a rare lesion characterized by mucosa with presence of lipid-laden macrophages in the lamina propria. Foam cells are CD68 positive lipid-laden macrophages without mucin or pigment.1 Foam cell aggregation including fat-loaded macrophages is observed in diverse conditions such as Whipple's disease, melanosis coli, malacoplakia, xanthogranuloma, hereditary metabolic storage disorder, and others.1 This disorder was first described as lipid islands by Lubarsch et al. after first found by Endo as yellow nodules composed of lipid deposition in gastric mucosa in 1910, and also called as gastric xanthoma, gastric xanthelasma and others.2
Several causes of gastrointestinal xanthomas have been hypothesized, and gastrointestinal xanthomas are mostly frequently detected in the stomach associated with chronic gastritis.3 Xanthomas are often occurred in the remaining part of the stomach after gastrectomy and is thought to be attributable to cell injury.2,4 Colonic xanthoma is also anticipated to occur due to cell damage generated by toxicity.5 Nakasono et al.1 assumed previous mucosal damage as the cause of colonic xanthoma and reported xanthomaotus polyps were frequently associated with proliferative epithelial cells, a thickening of the epithelial basal lamina, capillary proliferation, and others. No studies have been performed on colonic inflammation identified endoscopically and associated with colonic xanthoma.6 Despite the detection of foam cells, damages in epithelial cells of the rectal mucosa are nearly observed.7 Thus, colonic xanthomas are anticipated to occur during cellular regeneration rather than the processes of cell injury. Colonic xanthomas have so far only been detected in the sigmoid colon and rectum in recent case reports, and slow colonic transit time is thought to result in local mucosal damage.6
Coates et al.8 pointed out lipid metabolism abnormality as the cause of xanthomas since gastric xanthomas disappeared after treating hyperlipidemia detected in two patients. Nakasano et al.1 also suggested hyperlipidemia as the causal factor since 7 out of 25 patients with colonic xanthomas had hyperlipidemia. Isotomo et al.9 reported that gastric xanthomas were not related with diabetes mellitus, hypercholesterolemia, and skin lesions. According to Miliauskas et al.,6 serum lipid test revealed no hyperlipidemia in 9 patients among 13 patients with colonic xanthomas. Additional studies are thought to be crucial to further investigate the relationship with lipid metabolism. Since serum cholesterol level was not examined in this case report, the association with hyperlipidemia was not identifiable.
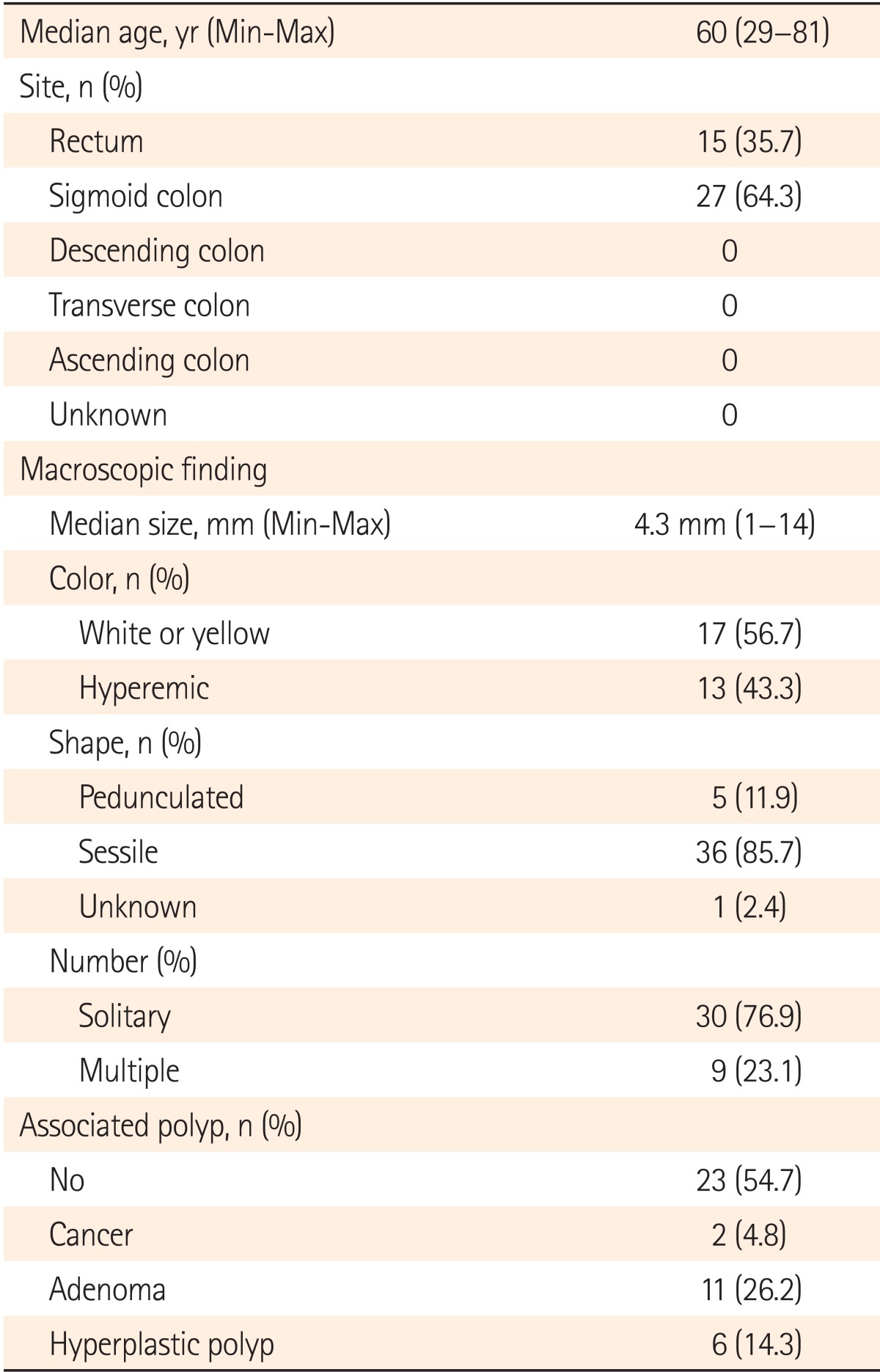
Gastrointestinal xanthomas are mostly found in the stomach5 and the prevalence of gastric xanthomas is reported to range between 1-4%.8 Although colonic xanthomas occur very rarely, 42 reported cases of colonic xanthoma were searched in English medical literature. All cases were rectosigmoid lesions (Table 1).1,6,10 Bejarano et al.7 diagnosed rectal xanthomas in two patients out of randomly selected 100 patients in their study. The actual prevalence of colonic xanthoma is anticipated to be higher. Diagnosis is difficult due to shape of xanthomas varying according to the size, density, mucosal state around lesion, and air pressure in colonoscopy with the naked eye. Biopsy is not recommended for a small hyperplastic polyp less than 5 mm in the rectal area where colonic xanthomas commonly occur.1
According to previous studies of Nakasono et al.1 and others (Table 1), colonic xanthomas were characterized by a mean size of 5 mm, sessile polyps (82.1%-85.7%), typically red (43.3%-60.0%) or white (25.0%-56.7%) in color. Only two xanthomas appeared yellow (7%). Unlike gastric and esophageal xanthomas, polyp-shaped non-yellowish color colonic xanthomas are known to be caused by capillary proliferation in the lower layer of epithelial cells.1
Since symptoms are hardly associated with colonic xanthomas, the lesions are commonly detected along with colorectal polyps during colonoscopy.6 Associated conditions of colonic xanthomas are adenomas (16%), adenocarcinomas (8%) and others adjacent to colonic xanthomas. Meanwhile, adenomas (12%), lesions and others are observed far from the location of colonic xanthoma.1 Up to now, adenomas (26.2%) and adenocarcinomas (4.8%) were detected in 42 cases, in addition to colonic xanthomas1,6,10 (Table 1). Moreover, fat accumulation in the colonic mucosa was suspected to be associated with the incidence of adenomas caused by the activity of protein kinase C in a previous study.11 A small-sized colonic adenoma was found in the opposite side of colonic xanthoma in this case report. Likewise, thorough examination of adenomas, adenocarcinomas and other lesions associated with and around lesions is crucial when colonic xanthomas are suspected during colonoscopic exam. Moreover, total resection is thought to be critical taking potential malignancy of lesions and its adjacent area into consideration.
This is the first reported case of colonic xanthoma expressed as LST in the ascending colon. This lesion was discriminated from LST with characteristics found on the surface shape and balloon-like swelling shape of skin lesions after submucosal injection. This is attributable to thin epidermis in colonic xanthoma in which the cause is the accumulation of foam cells in the lamina propria.
The authors detected a 15 mm sized red colonic xanthoma locally associated with white spots as a LST in the ascending colon. Taking into consideration the fact that this xanthoma could associate precancerous lesion, EMR was performed using a snare. In addition, small colonic adenomas were removed after thorough examination around the lesion. Therefore, we report this case with a brief review of literature.
Notes
Financial support: None.
Conflict of interest: None.