A patient presenting with abdominal pain radiating to the back
Article information

Question: A 76-year-old man visited our hospital complaining of abdominal pain of 2 months' duration. He presented with periumbilical pain radiating to the back. He had a medical history significant for diabetes mellitus, hypertension, bronchial asthma, and a cerebrovascular accident resulting in motor deficits on the right side of his body 8 years prior to hospitalization. He had not taken any medicines for treatment of tuberculosis.
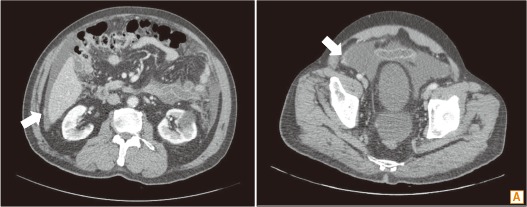
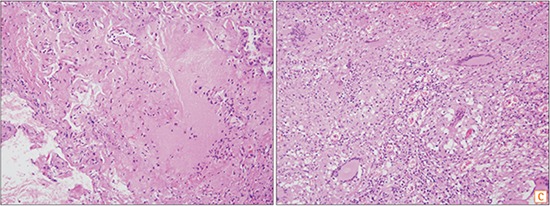
On admission, the patient's vital signs were within normal limits. Upon physical examination, the abdomen was distended with shifting dullness, and he exhibited mild tenderness in both sides of lower abdomen. Initial laboratory findings showed elevated CRP (5.12 mg/dL) and plasma fibrinogen (539 mg/dL) levels. Other laboratory findings were unremarkable as follows: white blood cell count, 8,290/mm3; hemoglobin level, 15.3 g/dL; platelet count, 302×109/L; levels of serum cholesterol, 145 mg/dL; serum total protein, 6.8 g/dL; serum albumin, 3.5 g/dL; serum total bilirubin, 0.5 g/dL; serum alanine aminotransferase, 15 IU/L; serum creatinine, 1.3 mg/dL; and BUN, 15 mg/dL; and prothrombin time 1.00 international normalized ratio. Findings on the chest radiograph were unremarkable. On the CT scan of the abdomen and pelvis, ascites with multifocal peritoneal thickening and enhancement was found, suggesting complicated ascites Fig. A, arrow). A diagnostic paracentesis revealed red blood cell count of 3,600/mm3, white blood cell count of 5,184/mm3, with 58% lymphocytes and 25% polymorphonuclear leukocytes, a serum ascites albumin gradient level of 0.8 g/L, and adenosine deaminase (ADA) level of 108 IU/L. On microscopic examination, no AFB were seen, and cytology examination results were negative for malignancy in the ascitic fluid. Ascitic fluid culture and PCR results for Mycobacterium tuberculosis were negative. Interferon-gamma release assay (IGRA) also revealed a negative result. However, the diagnostic laparoscopy demonstrated a thickened peritoneum with tubercle and ascites (Fig. B). On histologic examination of the peritoneal biopsy specimen, there was chronic granulomatous inflammation with caseous necrosis and multinucleated giant cells (Fig. C; H&E, ×200 [left], ×100 [right]). What is the most likely diagnosis?
Answer to the Images: Tuberculous Peritonitis
Tuberculous peritonitis is one of the most common types of extrapulmonary tuberculosis. It coexists with pulmonary tuberculosis in up to 3.5% of patients, and comprises 31%–58% of abdominal tuberculosis.1 Tuberculous peritonitis usually develops secondary to a hematogenous spread of tubercles from a pulmonary focus, although concomitant active pulmonary tuberculosis is rare.1 Many patients with tuberculous peritonitis present with abdominal pain (64.5%) that is frequently accompanied by abdominal distension and tenderness.1 Constitutional symptoms such as mild fever (59%) and weight loss (61%) are also common in tuberculous peritonitis.1 Ascites is present in about 73% of cases of tuberculous peritonitis.1 Ascitic fluid analysis should be performed routinely in all patients presenting with ascites. Most patients have white blood cell counts ranging between 500 and 1,500/mm3, with lymphocytic predominance and a serum ascites albumin gradient level of <1.1 g/dL.1
Delayed diagnosis is the most significant risk factor for high mortality in patients with tuberculous peritonitis.2 In spite of the clinical impacts of early diagnosis, tuberculous peritonitis remains a challenge for clinicians in countries with a high prevalence of tuberculosis because of the difficulty in diagnosing this condition. The gold standard for the diagnosis of tuberculous peritonitis is an ascitic fluid or peritoneal biopsy culture sample positive for M. tuberculosis. However, mycobacterial culturing has its limitations. It is time-consuming, as the results of mycobacterial cultures might take more than 4 weeks. It also has modest sensitivity of 66%–83%, even from as much as 1 L of ascitic fluid.1 Therefore, alternative non-invasive diagnostic tools, including Ziehl–Neelsen staining, PCR and ADA level in the ascitic fluid, and IGRA, are widely used for the rapid detection of tuberculous peritonitis. Unfortunately, AFB smears of the ascitic fluid are positive in only about 3% of the cases.1 PCR is a technique using nucleic acid amplification to detect M. tuberculosis, showing a disappointingly low sensitivity of 48% in smear-negative cases compared to excellent sensitivity in up to 95% of smear-positive cases.3 ADA level is elevated in tuberculous ascitic fluid because of T cells stimulated by the mycobacterial antigens. At present, an ADA activity of >30 IU/L is generally accepted as the cut-off level expected to provide the highest diagnostic yields for tuberculous peritonitis, with a sensitivity and specificity of >90%.1 Finally, interferon-gamma is a key cytokine of M. tuberculosis infection, involving recruitment of Th1 lymphocytes. IGRA, a quantitative assay evaluating the cell-mediated Th1 response to M. tuberculosis, had high sensitivity (93%) and specificity (99%) for detecting tuberculous peritonitis in a meta-analysis,4 despite the negative result in this case.
Laparoscopy is the diagnostic tool of choice in patients with suspected tuberculous peritonitis because it can be used to obtain peritoneal specimens for histology as well as to allow inspection of the peritoneum.1 Bhargava et al. classified the laparoscopic findings of tuberculous peritonitis into 3 types: a thickened, hyperemic peritoneum with ascites and whitish miliary nodules (66%; Fig. B); a thickened and hyperemic peritoneum with ascites and adhesions (21%); markedly thickened parietal peritoneum with possibly yellowish nodules and cheesy material along with adhesions (13%).5 Laparoscopy showed a high sensitivity of visual inspection, up to 93%.1 In addition, the presence of caseous necrosis provides the confirmative diagnosis of tuberculous peritonitis on the histologic exam of the peritoneal specimen. However, the morbidity and mortality associated with laparoscopy should be considered at the time of clinical decision, because the rates have been reported to be up to 5%.6
Notes
Financial support: None.
Conflict of interest: None.