Polypoid lesions at the anal canal: what do they hint?
Article information
Question: A 25-year-old man suffered from abdominal pain and fever in June 2015. He was admitted to the hospital nearby his home, where abdominal CT was done and showed the ascending and transverse colon colitis. Blood in stool was noted in July 2015. Therefore, colonoscopy was done and which disclosed ulcers at the terminal ileum and ascending colon. He lost 2.5 kg during that 1 month (his body weight decreased from 56.0 kg to 53.5 kg) and then remained stationary thereafter. Biopsy had been done and reported as erosions and chronic inflammation. He denied travel history, nor NSAID usage before that episode. Although no more abdominal pain nor blood in stool were noted after the discharge, he was referred to National Taiwan University Hospital for further management.
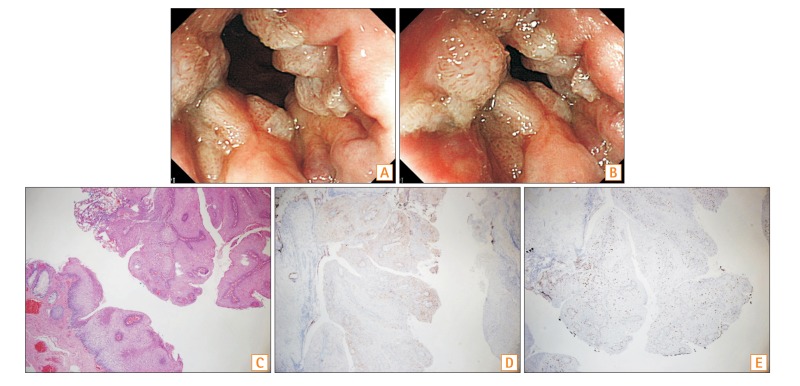
Colonoscopy was followed in October 2015, which showed only tiny erosions were noted at rectum and no more ulcers at the terminal ileum and ascending colon. Unexpected findings during the colonoscopy were the polypoid lesions at the anal area (Fig. A and B). What is your diagnosis for these polypoid lesions? And what kind of hint did they provide for you?
Answer to the Images: Anal Condyloma Acuminatum
Since anal condyloma was highly suspected, he was referred to the colorectal surgeon for further management. Transanal excision was done and histopathology study proved the diagnosis of condyloma acuminatum (Fig. C, H&E, ×40). Human papilloma virus type P16 staining was focal positive (Fig. D, ×40), and Ki-67 proliferation index was increased (Fig. E, ×40). He was reviewed again about the sex history and confirmed to have man with man anal sex, and he received human immunodeficiency virus (HIV) screening annually with all negative results.
Anal condyloma acuminatum is an infectious disease transmitted through sexual contact. The disease is caused by the human papillomavirus (HPV). Studies have found that men who have sex with men (MSM) demonstrate a higher prevalence of anal HPV infections. A multicity study of 1,218 HIV-negative MSM found a 57% prevalence of anal HPV infection.1 Recent research on perianal warts has revealed that high-grade intraepithelial neoplasia occurs in more than 50% of HIV-positive and up to 20% of HIV-negative men with perianal/anal warts.2 It has been recommended that all patients with perianal warts should have proctoscopy, and, ideally, all MSM and those who are HIV-positive should have biopsies prior to treatment. It is mandatory to follow up these patients carefully.3
Back to our patient, perianal observation is important while we performing the colonoscopy. Only when we pay attention and identify the clues that can help us for further diagnosis and management for patients with colitis. When anal/perianal warts identified, further sex history should be clarified. And, we should follow up the patient carefully since the risk of intraepithelial dysplasia/cancer increased in these patients.
Notes
Financial support: None.
Conflict of interest: None.