Cytomegalovirus colitis in immunocompetent patients
Article information
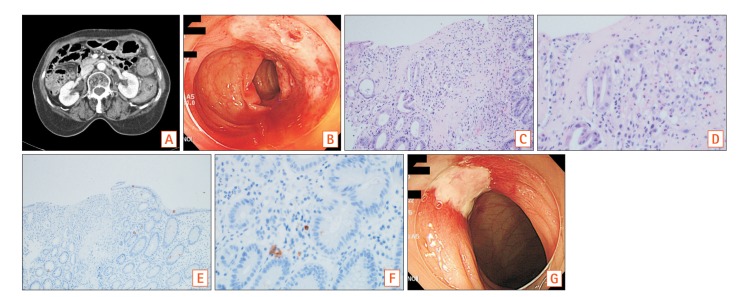
Question: A 63-year-old woman presented with left-sided abdominal pain and hematochezia noted over a week prior to hospitalization. She had been using antihypertensive medicine and did not report any other significant medical difficulties. A screening colonoscopic examination performed a year prior to presentation had been unremarkable. Abdominal CT showed segmental wall thickening with decreased enhancement of the proximal descending colon in addition to pericolic fat infiltration (Fig. A). Colonoscopic examination performed at Chungnam National University Hospital showed diffuse erythematous friable ulcerations located approximately 35 to 30 cm above the anal verge, and a biopsy was performed (Fig. B). Laboratory studies did not reveal any abnormalities including anti-human immunodeficiency virus antibodies.
What is the diagnosis of the ulcerative lesion in the colon?
Answer to the Images: Cytomegalovirus Colitis
Biopsy specimens were taken from the ulcerative lesions. Histopathological examination revealed atrophied crypts with cytomegalovirus inclusion bodies (Fig. C, H&E, ×200). The nucleus and cytoplasm of cells observed in the infected crypts were noted to be hypertrophied (Fig. D, H&E, ×400). Immunochemical examination showed positive nuclear staining for cytomegalovirus in an infected crypt (Figs E [×100] and F [×400], immunohistochemical staining).
Gastrointestinal (GI) involvement is usually secondary to the reactivation of latent infection in immunosuppressed patients. For example, patients who are treated with organ- or bone marrow-transplantation or are diagnosed with acquired immune deficiency syndrome, or those who use medicines such as immunosuppressants (anti-tumor necrosis factor antibodies, steroids) or chemotherapeutic agents. However, GI involvement is uncommon in immunocompetent patients. The cytomegalovirus (CMV) causes a variety of diseases in the lower GI tract such as colitis, ileitis, appendicitis, and colonic obstruction.123
The common presenting symptoms of CMV colitis are diarrhea, fever, abdominal pain, and approximately 50% of the patients demonstrate hematochezia.4
In a retrospective study comprising immunocompetent patients diagnosed with CMV colitis, the most common endoscopic findings were: well-demarcated ulcerations (50%), ulceroinfiltrative changes (25%), and pseudomembrane formation (25%).5
It is necessary to differentiate between CMV and ischemic colitis when an elderly patient presents with bloody diarrhea and abdominal pain.
Currently, the drugs available for treatment of CMV infection include ganciclovir, valganciclovir, foscarnet, and cidofovir. In immunocompetent patients diagnosed with CMV infection, ganciclovir is the most preferred antiviral drug. After a definitive diagnosis of CMV colitis, our patient was treated with intravenous administration of ganciclovir at a dose of 200 mg per 12 hours for 2 weeks. A follow-up colonoscopic examination showed improvement in the colonic ulcers (Fig. G) and disappearance of the CMV inclusion bodies and CMV-positive cells.
CMV enteritis in immunocompetent patients may occur in elderly patients or in those with a concomitant underlying disease. CMV colitis results in poor outcomes without the administration of antiviral treatment. Antiviral therapy is recommended for the management of immunocompetent patients. The prognosis is relatively good if the condition is promptly and correctly diagnosed and treated.6
Notes
FINANCIAL SUPPORT: The authors received no financial support for the research, authorship, and/or publication of this article.
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION: Jae Ho Park wrote the manuscript, processed the images and pathologic findings.
Hee Seok Moon selected case and reviewed the final version of the manuscript.