Does Carotid Intima-Media Thickness Increase in Patients With Inflammatory Bowel Disease?
Article information
Abstract
Background/Aims
Mesenteric microvascular thrombosis has been implicated as a contributing factor to the pathogenesis of inflammatory bowel disease (IBD). The aim of the current study was to assess the possibility of subclinical atherosclerosis in patients with IBD by measuring their carotid intima-media thickness (c-IMT).
Methods
Thirty-eight patients with IBD who were followed-up for at least 3 years participated. Patients with a history of cardiovascular disease and known risk factors for atherosclerosis were excluded. As a control group, 38 healthy patients matched for age and gender without atherosclerosis risk factors were included. Carotid ultrasonography was performed in all patients and controls. Patient baseline characteristics and laboratory parameters were recorded to evaluate atherosclerosis risk factors.
Results
The mean age of patients with IBD was 38.5±6.62 years. Twenty-three patients with IBD were diagnosed with ulcerative colitis and the other 15 cases were diagnosed with Crohn's disease. The median duration of disease was 52.0 months. Serologic markers such as erythrocyte sedimentation rate, C-reactive protein (CRP), and cholesterol levels differed significantly, however, there was no significant difference in c-IMT between patients with IBD and those in the control group (0.53±0.10 mm vs. 0.53±0.07; P=0.85). Multivariate analysis revealed that body mass index, CRP, disease duration, and age were significantly correlated with c-IMT in patients with IBD.
Conclusions
The results of the current study did not show an increase in c-IMT in patients with IBD. Further studies that include more subjects and a longer follow-up period will be necessary in order to evaluate the risk of atherosclerosis in Korean patients with IBD.
INTRODUCTION
The etiology of IBD, a chronic intestinal inflammation, has not been elucidated. Environmental, genetic, and immunologic factors, as well as microvasculature abnormalities, may be associated with the pathogenesis of the disease, and abnormal intestinal immune responses result in inflammation in patients with genetic susceptibilities.1,2,3 Several chronic systemic inflammatory diseases, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), are associated with the development of atherosclerosis.4,5 In these diseases, atherothrombotic complications are among the most important causes of mortality and morbidity.5 Strong evidence of accelerated atherosclerosis in patients with IBD may be of significant clinical relevance and would therefore necessitate screening in patients with long-standing IBD in order to prevent atheroembolic complications.
Recently, various non-invasive markers of arterial wall alteration have been used in clinical settings. These markers include carotid intima-media thickness (c-IMT), homocysteine, and insulin resistance.6,7 Among them, c-IMT measurement by ultrasonography is a relatively simple, safe, inexpensive, and reproducible measure that correlates well with cardiovascular risk factors.8,9 Currently, c-IMT is most commonly used to assess emerging atherosclerosis risk factors.
Evidence for an association between atherosclerosis and IBD is mixed. Additionally, all studies conducted on the subject to date have been derived from Western countries.10,11,12 Based on this background, the current study was conducted in order to assess the possibility of subclinical atherosclerosis in patients with IBD by measuring their c-IMT.
METHODS
1. Patients
Of the 247 patients with IBD in our institution, 136 patients <45 years of age were considered for inclusion. Patients who had atherosclerotic diseases including cardiovascular, cerebrovascular, and peripheral artery disease, or known risk factors such as hypertension (defined as blood pressure >140/80 or under treatment), hypercholesterolemia, diabetes mellitus, smoking, heart failure, pregnancy, obesity, and age ≥45 years were excluded. Among them, 38 patients with IBD who were followed-up for at least 3 years were included in the study.
An additional 38 cases who had visited our health promotion center were matched with the patient group by gender and age to serve as healthy controls. Because some of the patients with IBD were of extremely low body weight and height, control subjects with a matching BMI were unavailable. Therefore, patient and control groups were not matched for BMI. Control subjects lacked known risk factors and did not have atherosclerotic disease.
The medical records of 76 subjects were reviewed retrospectively after securing informed consent. The baseline characteristics of all subjects, including blood pressure, height, and weight, were collected, as well as information pertaining to IBD such as diagnosis, duration, disease activity, and treatment.
The study was approved by Yeungnam University Hospital institutional review board in accordance with the Helsinki Declaration.
2. Laboratory Tests and Measurement of c-IMT
Laboratory testing was performed after a 12-hour fast. Tests included a lipid battery (total cholesterol, triglycerides, LDL cholesterol, and HDL cholesterol) and total glucose measurement. Inflammatory markers such as CRP and the ESR were also assessed.
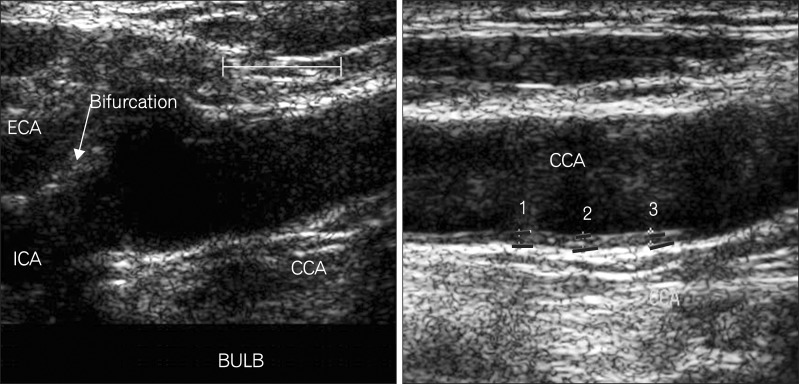
The carotid arteries were assessed using high-resolution B-mode ultrasonography (Acuson, Mountain View, CA, USA) with a 7 MHz linear transducer by 1 sonography technician who was unaware of the patients' clinical histories. Patients were examined in the supine position with the neck rotated 45° in the direction opposite to the site being examined. c-IMT was measured in accordance with methodology described in the published guidelines6 and evaluated on the far wall at 5, 10, and 15 mm proximal to the carotid bifurcation over both common carotid arteries. c-IMT was calculated by measuring the distance between the leading edge of the lumen-intimal interface to the leading edge of the media-adventitia interface of the far wall at the distal wall of the carotid artery (Fig. 1). The final c-IMT value represented an average of the 6 c-IMT results from the left and right sides. The time interval between measurement of c-IMT and performance of laboratory tests was within 1 week.
3. Statistically Analysis
All data were expressed as the mean±SD or median for continuous variables. Categorical variables were the number of patients and the percentage in each group. Cross-tabs and descriptive procedures were used to analyze frequencies of categorical variables. Because there were no data available on the c-IMT of patients with IBD, the number of patients and controls needed in order to achieve statistical significance was determined based on a study of RA (β=0.10 and α=0.05).13 Continuous variables were compared using paired t-tests and chi-square tests with Fisher's exact correction applied to evaluate differences for categorical variables as necessary. A stepwise linear regression procedure was used to assess the correlation of various factors with increased c-IMT. Because we could not match patients and controls for BMI, analysis of covariance was used with BMI as a covariate. Values of P<0.05 were considered statistically significant and SPSS software (SPSS, Chicago, IL, USA) used for all statistical analyses.
RESULTS
1. Baseline Characteristics of the Study Subjects
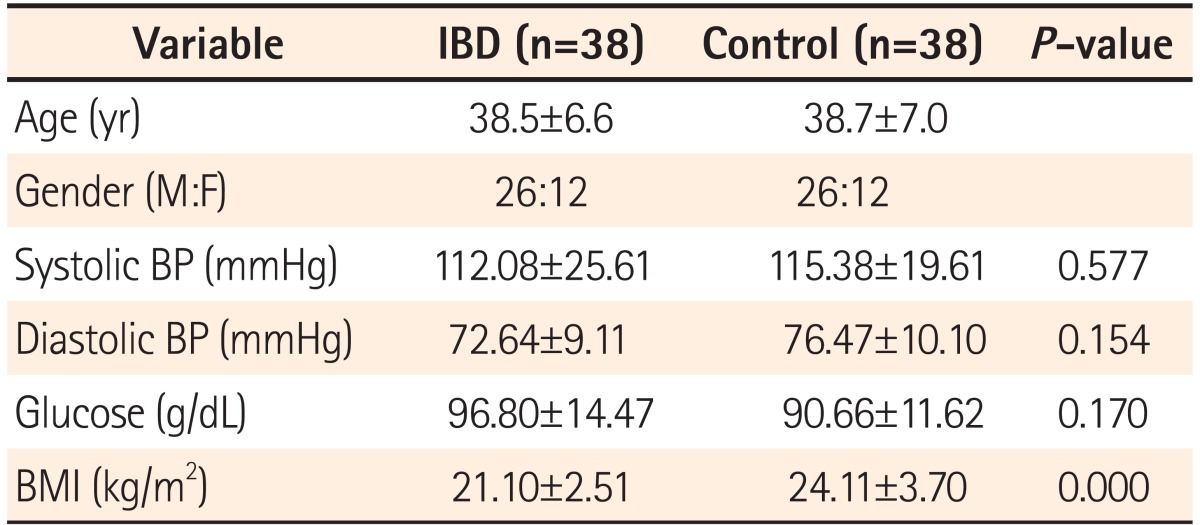
The mean ages of patients with IBD and healthy controls were 38.5±6.6 years and 38.7±7.0 years, respectively. The male-to-female ratio was 26:12 in both groups. With the exception of BMI, all other parameters did not differ significantly between patients with IBD and healthy controls. The mean BMI of healthy controls (24.11±3.70) was significantly higher compared to patients with IBD (21.10±2.51; P=0.00) Systolic and diastolic blood pressures were within normal limits in both groups. Fasting blood sugar levels were 96.8±14.5 g/dL and 90.7±3.7 g/dL in the patient and control groups, respectively (Table 1).
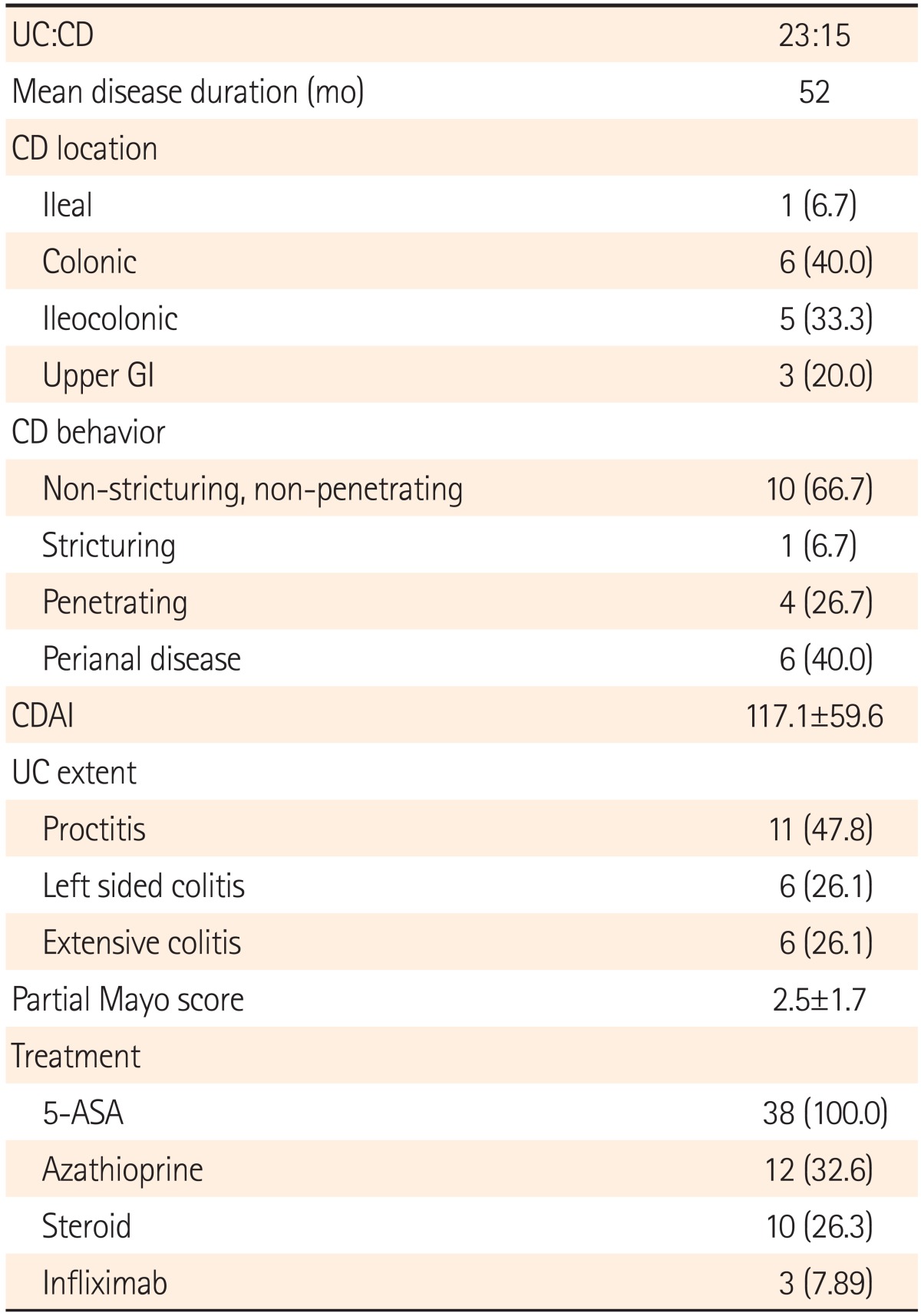
Among the 38 patients with IBD, 23 were diagnosed with UC and 15 were diagnosed with CD. The median duration of disease was 52.0 months. Among patients with CD, 40% of the cases were colonic involvement, ileocolonic in 33.3%. Inflammatory type is the most common behavior of CD (10 cases, 66.7%) and perianal involvement was noted in 6 cases (40%). The mean CDAI at the time of c-IMT measurement was 117.1±59.6. Eleven cases of UC was involved in rectum (47.8%) and the partial Mayo score was 2.5±1.7. All patients with IBD were taking 5-aminosalicylic acid. In addition, azathioprine or prednisolone was used in 12 and 10 patients, respectively. Infliximab was used in 3 patients with CD (Table 2).
2. Comparison of c-IMT and Clinical and Laboratory Variables
Mean blood levels of several serologic markers associated with inflammation showed a significant difference. ESR and CRP were significantly higher in the IBD group (both P=0.00). Lipid profile results revealed that total cholesterol, HDL cholesterol, and total glucose were all significantly higher in the control group (Table 3).

Comparison of Carotid Intima-Media Thickness (c-IMT) and Serologic Markers for Inflammation Between the IBD and Control Groups
The mean c-IMT was 0.531±0.097 mm in the IBD group and 0.535±0.072 mm in the control group. Plaques were detected in 6 study subjects, 2 of whom were in the IBD group. c-IMT did not differ significantly between groups (P=0.85) and this result did not change after adjusting for BMI. In an analysis of only the 20 patients whose BMI could be matched to a control, the mean c-IMT of the IBD patients was higher but without statistical significance (0.540±0.095 vs. 0.538±0.076; P=0.91). Among patients with IBD, c-IMT did not differ between patients with CD and UC. Furthermore, c-IMT did not show significant differences between those with and without plaques (Table 3).
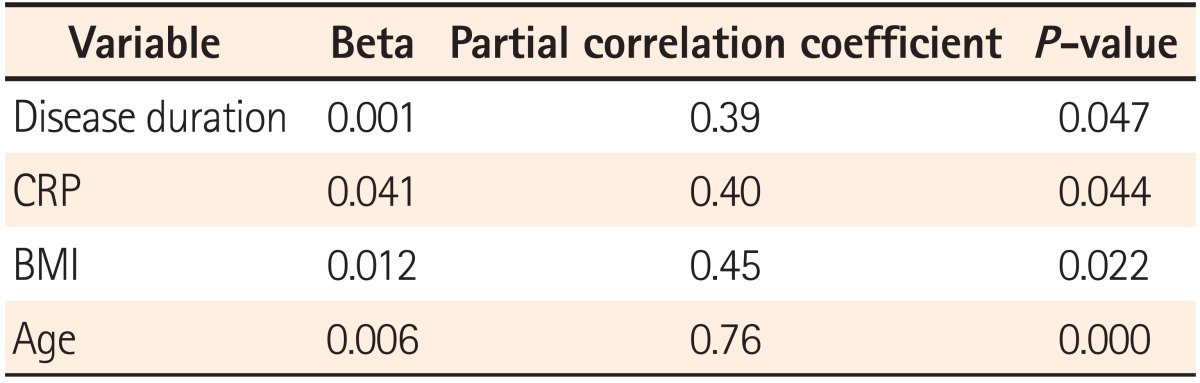
A multivariate analysis using linear regression was performed to assess the factors correlated with c-IMT in patients with IBD. Long disease duration, high serum CRP levels, lower BMI, and old age were significantly associated with increased c-IMT (Table 4). However, disease severity was not a significantly associated factor.
DISCUSSION
Although the mechanisms underlying the pathogenesis of IBD have not been elucidated fully, it is possible that an uncontrolled immune response may give rise to chronic inflammation of the intestines.1,2 It is important to note that chronic inflammation has been associated with cardiovascular disease14,15 and that these findings have been reported from patients with SLE2 and RA.15,16,17 However, the occurrence of early atherosclerosis in patients with IBD differs between studies conducted in Western countries. It is therefore of great importance to clarify the risk of atherosclerosis in chronic intestinal inflammation due to the relatively young age of most patients with IBD and the devastating results of atherosclerosis. There have been no comparable studies of Asian patients with IBD, including Koreans. In the current study, we assessed the possibility of early atherosclerosis in Korean patients with IBD.
A great deal of research interest has been focused on discovering predictive markers of early atherosclerosis as indicators of cardiovascular events. Although their influence differs, known parameters include insulin resistance, c-IMT, hyperhomocysteinemia, CRP, and coronary calcification.9,10,18,19,20 Among them, c-IMT can be assessed with relative ease and safety using ultrasound. In addition, the test is inexpensive, precise, and reproducible.8 For these reasons, it has become one of the most widely used methods in clinical research to evaluate the risk factors of atherosclerosis. Reports have chronicled positive associations using c-IMT21,22 and implicated c-IMT as a strong predictor of both myocardial infarction and stoke.9
The normal value of c-IMT is highly dependent on the methodology employed, as well as the age and gender of the examinee.7,23,24 The normal ranges for those <30-, 31-40-, 41-50-, and >50-years-of-age are 0.44-0.57 mm, 0.42-0.5 mm, 0.44-0.57 mm, and 0.46-0.7 mm, respectively. However, since c-IMT is considered as a candidate marker of cardiovascular risk, the current epidemiological data indicate that a c-IMT ≥1 mm at any age is associated with significantly increased risk.7 In the current study, we measured the distance by manual cursor placement at multiple sites. In some cases, the plaque-presenting site could be measured. However, c-IMT was not significantly higher in cases of plaque. This may have reflected the very small number of patients in whom plaque was detected.
In our study, the c-IMT in patients with IBD was not significantly higher than that of controls matched for other characteristics, with the exception of BMI. Because the control group data were selected from patients who visited our health promotion center, we could not match BMI exactly. Some of the patients with IBD had an extremely low BMI, making it very difficult to obtain matched controls. This may have affected the results, however, the finding that the results did not change after adjustment for BMI suggests that there may be other factors associated with c-IMT. This result is consistent with the results obtained from several Western studies,25,26,27 although it is inconsistent with at least one study.11
Serologic markers such as ESR and CRP were significantly higher in the IBD group than in the control group. This indicates that IBD patients are more exposed to an inflammatory condition than controls despite the long-term use of anti-inflammatory medications. However, for reasons that remain unclear, the c-IMT of patients with IBD was not higher than that of controls. Explanations may include the low BMI in our patients with IBD, the relatively short duration of follow-up, the possibility of genetic differences from Western patients, and the co-existence of a protective effect against atherosclerosis.
Considering that obesity is a known risk factor for atherosclerosis,28 it is not surprising that the lower BMI of patients with IBD was associated with a lack of increased c-IMT. The duration of studies of other chronic systemic inflammatory disease such as RA and SLE was longer than in the current study,4,29 suggesting that a longer follow-up of patients with IBD is warranted. Recent epidemiologic and genetic studies have reported several differences between Korean and Western patients with IBD. In Koreans, the severity of IBD was relatively more mild than that seen in Western patients.30,31 The risk of atherosclerosis in Korean patients with IBD may be very low and possibility attributable to genetic factors associated with effective protection.
In the present study, the factors that correlated with c-IMT were older age, longer disease duration, higher levels of CRP, and lower BMI levels. These factors were all positively correlated with c-IMT. The results of the current study are consistent with the results of a study that examined factors related to c-IMT.6 Several studies have suggested that homocysteine is a factor that correlates with c-IMT.6,26 However, we could not assess this parameter, as members of the control group were not checked routinely for homocysteine. In patients with IBD, disease severity was not found to be a correlating factor. Because the natural course of IBD waxes and wanes, it might be difficult to extrapolate the severity measured at any particular time point over the entire course of the disease. However, the disease duration in patients with IBD correlated positively with c-IMT. Because we excluded patients or controls who had well-known risk factors for atherosclerotic diseases (hypertension, family history, smoking, and dyslipidemia), and matched for age, disease duration may have an independent role in the development of atherosclerosis.
The current study had several limitations. First, we could not assess various inflammatory markers and could not match BMI exactly in the control group. Second, the disease duration may have been too short to detect differences. Considering that disease duration correlates positively with c-IMT, continuous patient follow-up would seem prudent.
In conclusion, c-IMT as a marker for early atherosclerosis did not increase in patients with IBD in our study, although the results may have been affected by the aforementioned limitations. Long disease duration, CRP, high BMI, and old age showed positive correlations with c-IMT. This is the first study to assess the risk of atherosclerosis in Korean patients with IBD using c-IMT. To clarify the risk of atherosclerosis in Korean patients with IBD, studies including larger numbers of patients with a longer follow-up duration would need to be conducted.
Notes
Financial support: None.
Conflict of interest: None.