What's the Clinical Features of Colitis in Elderly People in Long-Term Care Facilities?
Article information
Abstract
Background/Aims
As life expectancy has increased, the number of elderly patients who need long-term care has grown rapidly. Mortality in patients with colitis in long-term care facilities (LTCFs) is increasing. We intend to investigate the main causes of colitis in LTCFs compared to those of colitis in local communities, and to identify the clinical features and risk factors of patients with colitis in LTCFs.
Methods
We retrospectively analyzed epidemiology, medical conditions, laboratory values, diagnoses, and clinical courses of elderly patients aged ≥65 who were admitted to the Ewha Womans University hospital with colitis between January 2007 and July 2012.
Results
Patients with colitis in LTCFs (n=20) were compared with elderly patients with colitis in local communities (n=154). Fifty-five percent of colitis in LTCFs was caused by Clostridium difficile infection (CDI), 30% was due to ischemic colitis, and 15% was due to non-specific colitis. Non-specific colitis was the most common (63%) in the community group. Clinical outcomes were also significantly different between both groups: higher mortality (10.0% vs. 0.64%, P=0.021), higher requirement for intensive care units care (50.0% vs. 18.8%, P<0.01) in LTCFs group. In univariate analysis, the most significant risk factor for death in patients in LTCFs was decreased mental faculties.
Conclusions
Patients in LTCFs showed worse clinical outcomes and a much higher prevalence of CDI compared to patients from local communities. We suggest early and active evaluation, such as endoscopic examination, for differential diagnosis in patients in LTCFs.
INTRODUCTION
With life expectancy rising thanks to recent advances in medicine, the numbers of elderly patients who require long-term care is also increasing. This means that care requirements for elderly people are also greater. Along with the fastest rate of aging in the world, the Korean government's policies for the expansion of long-term care facilities (LTCFs) have been implemented in parallel with increased geriatric diseases, which have led to an increase in the number of patients in these facilities, with an approximately 50-fold increase compared to 2000.
Elderly patients are generally characterized by reduced immune function, and patients in LTCFs often have reduced defense mechanisms because of secondary issues including malnutrition, multiple chronic diseases, and combined medications, which make them susceptible to diseases, especially infectious diseases.1,2 Several investigations are currently ongoing worldwide, including the USA, with respect to the epidemiology as well as policies for the management and prevention of infectious diseases due to considerable numbers of patients in such facilities with malfunctions (e.g., fecal or urinary incontinence) and difficulties in hygiene management owing to impaired cognitive ability and mobility.3,4 On the other hand, in South Korea, more studies are warranted given the fact that (1) increasing numbers of patients are being transferred from facilities (i.e., LTCFs) to higher-tier hospitals and (2) mortality in patients who are under is increasing.
Gastrointestinal symptoms including diarrhea are commonly found in elderly patients, and more patients are being transferred to higher-tier hospitals, such as tertiary hospitals, for treatment. In particular, the mortality of colitis patients who are staying in LTCFs is as high as 17.5%;5,6 one study has indicated that it could be elevated by up to 4 times in patients from local communities.7 In addition, because of the frequent use of antibiotics, the incidence rate of Clostridium difficile infection (CDI) has been increasing sharply8, and it has been pointed out that long/short-term hospitalization in such facilities, as well as increases in the numbers of elderly patients, are critical risk factors9,10, yet epidemiological studies and management for patients in Korea are scarce. In this study, we investigate the risk factors of mortality and causes/clinical properties of colitis via comparison with colitis found in local communities in order to improve the determination of prognosis as well as proper treatment for colitis patients in LTCFs.
METHODS
1. Subjects
Of all patients transferred into the Ewha Womans University Mok-dong Hospital with diarrhea, bloody stool, and abdominal pains from LTCFs between January 2007 to July 2012, we analyzed patients who (1) were hospitalized via the emergency room (ER) (2) stayed in a long-term care facility for longer than a week. A total of 20 patients were selected who were diagnosed with colitis based on examinations of medical history, clinical symptoms, blood tests, stool examinations, and endoscopy and radiology findings. When it came to subject selection, we chose subjects for whom more than one typical clinical symptom was addressed such as diarrhea, bloody stool, and abdominal pain, yet medical history and radiology examinations including abdominal CT performed in the ER were utilized to confirm causes of symptoms, i.e., other than colitis, in order to exclude subjects. Endoscopy was mainly performed for differential diagnosis, and colitis included various lesions such as serious bleeding, flare and edema of the colonic mucosa, and exudation, while stool examinations were implemented in order to identify causative organism(s) if infectious diseases were suspected. The exclusion criteria were (1) patients with organic gastrointestinal disorders such as IBDs, tuberculosis, and gastrointestinal cancers, (2) diagnosis was unclear as colonoscopy was not performed, and (3) causes of diseases were not confirmed since other infection factors were present. For the control group, we selected hospitalized patients from local communities who were >65 years old, and hospitalized mainly because of diarrhea, bloody stool, and abdominal pain in the same period; in addition, for all patients diagnosed with acute/chronic colitis, identical exclusion criteria were applied as for patients from LTCFs, producing a final cohort of 154 patients for analysis and comparison.
2. Methods
The present study was performed via a retrospective review of patients' medical data, and eligible patients who met all inclusion criteria were investigated with respect to their age, sex, medication history, length of stay in LTCFs, symptoms, and duration of symptoms before they visited the ER, level of awareness, and underlying diseases. In order to exclude organic causes and to diagnose colitis, stool examinations, blood tests, endoscopy findings, and radiologic images were comprehensively analyzed, and medications, mortality rates during treatment, ratio of hospitalization in intensive care units (ICUs), and duration of hospitalization were examined to determine clinical progress and prognosis.
Depending on the cause, colitis was classified into several groups and diagnostic methods as follows: pseudomembranous colitis was diagnosed and classified into CDI when typical characteristics were found, namely slightly elevated, yellow or white, well demarcated 2-5-mm plaques overlying the edematous mucosa. CDI was diagnosed in cases where (1) no pseudomembranous lesion was observed by endoscopy, (2) patients had a history of antibiotic usage as well as clinical symptoms, and (3) C. difficile toxin was detected in stool examinations utilizing enzyme immunoassays (i.e., toxin A/B), or the organism was isolated by a feces culture test. Although there is no clear criterion for ischemic colitis, it was primarily diagnosed based on the history of underlying diseases that may cause ischemic colitis, symptoms accompanying bloody stools, endoscopic visual appearance, and lesion area. In addition, endoscopic biopsy was utilized to finalize the diagnosis of ischemic colitis. Infectious colitis was determined as non-specific colitis, and some was classified as other causes after excluding organic gastrointestinal disorders, ischemic colitis, and CDI in which colitis was found on colonoscopy, medical history, and clinical symptoms. Although infectious colitis is caused by bacteria, viruses, parasites, and fungi, it is not easy to definitely diagnose infectious colitis because of given that less than 50% of cases reveal a causative organism in stool culture tests.11 Most infectious colitis was found to be acute and accompanied by watery diarrhea and fever; it is known to be caused by contaminated foods and water hence, we identified this via clinical characteristics and medical history analysis. In cases of subacute or chronic colitis, we monitored mucosal appearance (e.g., mucosal edema, flare, bleeding spots, erosions, ulcers) and lesion areas through colonoscopy and confirmed endoscopic biopsies, then made a diagnosis of infectious bowel disease/intestinal tuberculosis.
Even though organ transplant or cancer patients with reduced immune function may have elevated risks of infection, patients with colitis due to immunological abnormalities and systematic diseases were classified as having non-specific colitis since it is difficult to find a consensus on examination. The present study was performed with the approval of the institutional review board of the Ewha Womans University Mok-dong Hospital (IRB file No. 2014-04-013).
3. Statistical Analysis
All data in the present study were analyzed utilizing IBM SPSS Statistics version 20 (IBM Co., Armonk, NY, USA). Descriptive statistical data were expressed as means±SDs or percentages (%), and categorical variables and continuous variables were analyzed via the Pearson's chi-square test and Student's independent t-test, respectively. Univariate analysis was performed to assess the risk factors responsible for the mortality rate of colitis patients in LTCFs. A P-value <0.05 was considered to be statistically significant.
RESULTS
1. Clinical Characteristics of Study Subjects
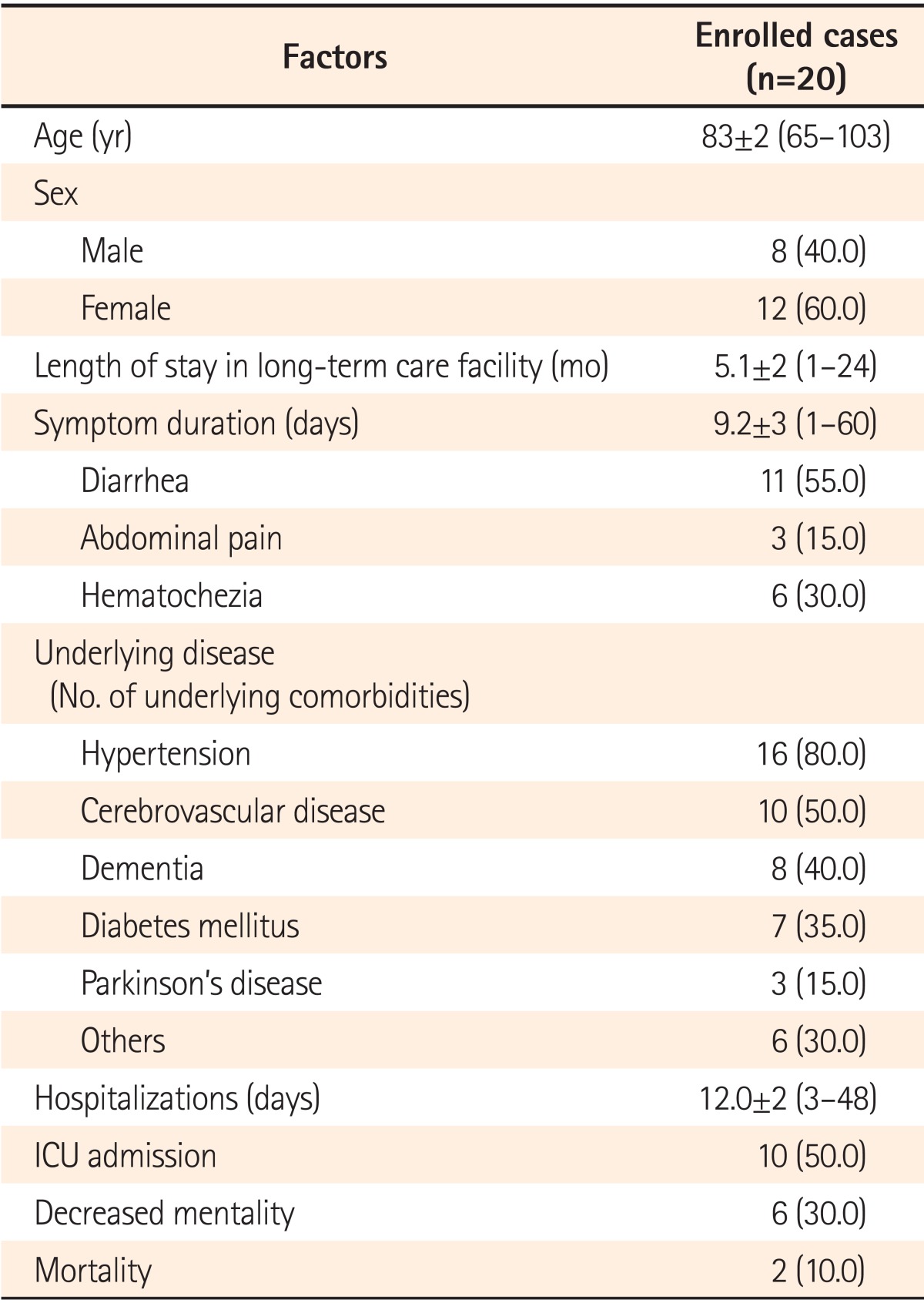
A total of 20 patients were transferred from LTCFs with a mean age of 83±2 years (range, 65-103 years); female patients outnumbered (12 female patients; 60.0%) male patients. The average length of residence in LTCFs was 5.1 months (range, 1-24 months). Major symptoms were diarrhea (11 patients; 55.0%), followed by bloody stool (6 patients; 30.0%), and abdominal pain (3 patients; 15.0%). The average period for symptom complaint, defined as the time between the occurrence of symptoms and hospitalization, was 9.2±3 days (range, 1-60 days) on average. Of all patients, 16 (80.0%) had accompanying hypertension, while other underlying diseases were cerebral infarction (10 patients; 50.0%), dementia (8 patients; 40.0%), diabetes mellitus (7 patients; 35.0%), and Parkinson's disease (3 patients; 15.0%); overall, patients tended to have more than two diseases. Before admission, patients were medicated with blood pressure medications, blood glucose lowering drugs, aspirin and anti-platelet agents, and anti-thrombotics for their underlying diseases; although gastric mucosal protective agents were being used in combination with other medications, no patient was taking gastric acid suppressants. A total of 10 patients had a history of antibiotic medication and all of these patients were diagnosed with CDI. In terms of antibiotic types, cephalosporin was the most frequently utilized (i.e., 7 patients), followed by aminoglycoside, quinolone, and penicillin (2 cases each). Six patients were simultaneously medicated with more than two antibiotics. The average duration of hospitalization was 12.0±2 days (range, 3-48 days), and 50.0% of patients visited the hospital with severe conditions requiring ICU admission. Six patients with decreased mentality accompanied by clouding of consciousness were found; two patients with pseudomembranous colitis (10.0%) passed away due to septicemia (Table 1).
2. Comparison of Colitis Occurrence Between Local Community and LTCFs
Depending on the cause, colitis was classified as CDI, ischemic colitis, non-specific colitis, and "other". As described above, CDI and ischemic colitis were diagnosed in cases where the aforementioned criteria were met, while patients with non-specific colitis represented infectious colitis, excluding CDI, and included cases accompanied by conditions of systematic diseases (e.g., immune diseases with unknown causes and vasculitis). In stool/biopsy examinations, we found that causative organisms were C. difficile, Entamoeba ihistolytica, and cytomegalovirus. Other categories included diverticulitis, radiation enteritis, solitary rectal ulcer syndrome caused by physical stimuli, and colitis by causative agents (e.g., laxatives, and anti-cancer agents), with diverticulitis (6 patients), and radiation enteritis (4 patients) being the most common.
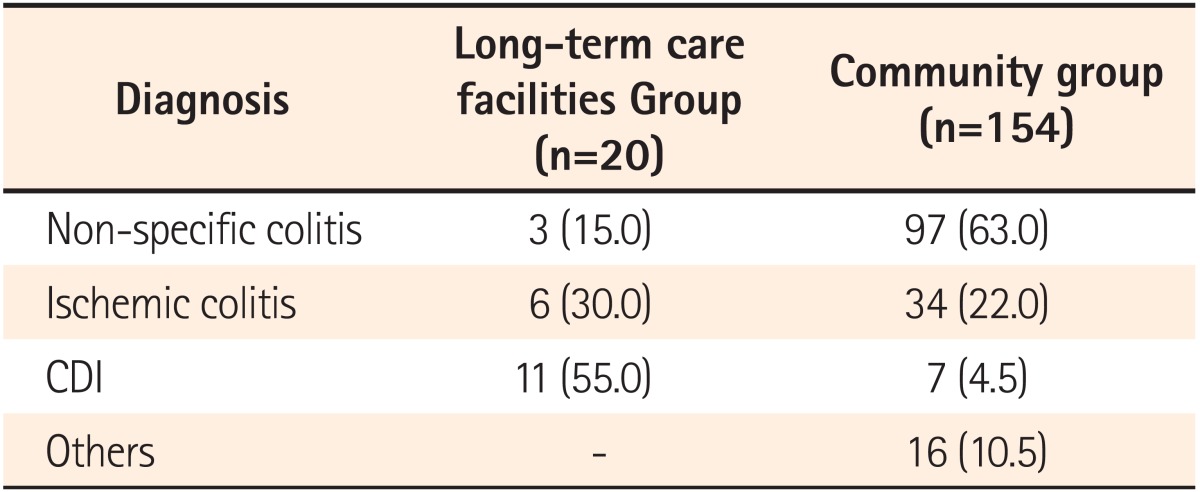
In the study group (i.e., LTCFs group), 11 patients (55.0%) were diagnosed with CDI, which was the most prevalent, followed by ischemic colitis (30.0%), and non-specific colitis (15.0%). In contrast, in the local community group, 63.0% of patients were diagnosed with non-specific colitis, followed by ischemic colitis (22.0%), and other causes (10.5%). We noted that CDI was found to be the least frequent (seven patients, 4.5%) (Table 2).
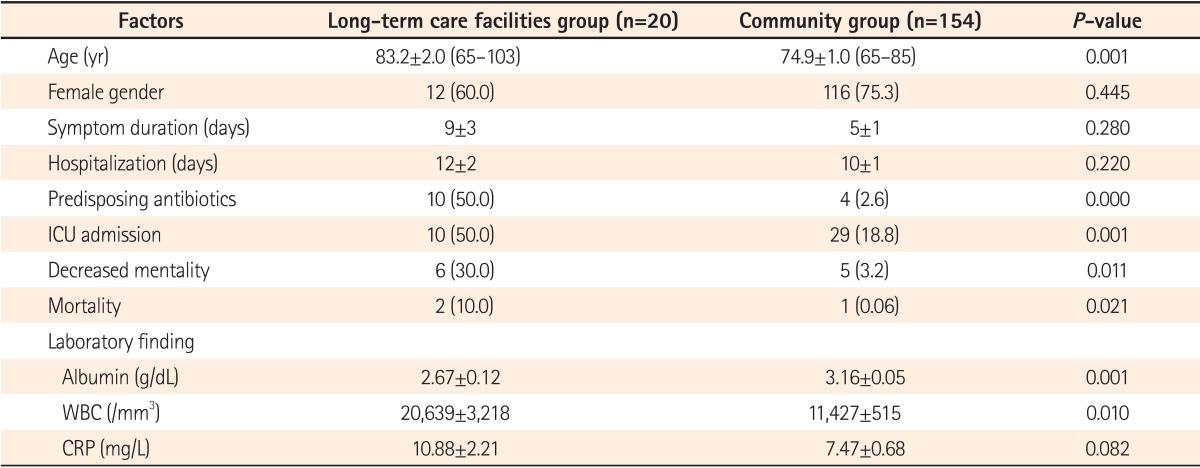
In terms of clinical characteristics, the average age was higher in the LTCFs group (83.2 years vs. 74.9 years, P=0.001), yet female patients outnumbered male patients in both groups. Although the duration of symptoms and hospitalization was slightly longer in the LTCFs group, no statistically significant difference was noted. History of antibiotic use was more prevalent in the LTCFs group, possibly due the greater number of patients with CDI. Ratio of ICU admission was significantly higher in the LTCFs group compared to the local community group (50.0% vs. 18.8%, P=0.001). Similarly, decreased mentality (30.0% vs. 3.2%, P=0.011) and mortality rate (10.0% vs. 0.06%, P=0.021) were higher in the LTCFs group compared to the local community group. In terms of blood test results, albumin levels were significantly lower (2.67 g/dL vs. 3.16 g/dL, P=0.001) while white blood cell (WBC) counts were higher in the LTCFs group than in the local community group (20,639/mm3 vs. 11,427/mm3, P=0.010) (Table 3).
3. Analysis of Risk Factors Utilizing Mortality
Univariate analysis was performed to assess risk factors responsible for mortality in colitis patients in LTCFs; none of the risk factors was shown to be significant except for decreased mentality (OR, 1.750; 95% CI, 1.167-4.648) (Table 4).
DISCUSSION
The majority of infectious diseases in patients in LTCFs are urinary tract and respiratory infections, closely followed by colitis and skin infections. It has been reported that of all cases of infectious disease, 49% require the administration of intravenous antibiotics, while 30% of patients should be transferred to higher-tier hospitals for acute care.3,12 There are several explanations for the increase in occurrences of colitis in LTCFs; specifically, reduced immunity and gastric acid secretion due to aging, as well as increased chances of infections (e.g., human-mediated infections and food borne infections) owing to public facilities such as rehabilitation clinics, bathrooms, and dining rooms might be responsible for this trend.13,14 In other countries, nursing facilities have managed the problem systematically; according to large-scale epidemiological studies regarding the management of such facilities, 52% of colitis was caused by food. Bacterial and viral infections account for 31% and 69% of colitis, respectively.15 The norovirus was found to be the most frequent causative organism, followed by C. difficile, Salmonella, Escherichia coli, and Shigella.13,16
In the present study, CDI was the most frequent cause of colitis in patients who were transferred from LTCFs (55.0%); in cases of death, all patients were diagnosed with CDI, confirming that severe CDI represents an unfavorable prognosis compared to other types of colitis given that no cases of death were noted in patients with infectious colitis or ischemic colitis. It has been reported that colonization of C. difficile might be found in 2% of healthy adults, and can be increased by 4-20% in patients in nursing facilities. It varies dramatically by country and age; one report showed that 46% of patients who were residing in such nursing facilities were colonized by C. difficile.17,18,19 In South Korea, an epidemiological study mainly investigating university hospitals also indicated that the occurrence rate of CDI was increased.20 Major explanations for the high occurrence rate of CDI in patients in LTCFs include (1) acquisition of new causes of diseases due to a history of frequent hospitalization, (2) ease of propagation by direct contact, (3) medications that are known risk factors for infections, and (4) underlying disease conditions; of these, exposure to frequent antibiotics might be the most critical cause.8,21,22
Upon exposure to antibiotics, the normal intestinal microorganisms can be destroyed, thereby leading to colonization by C. difficile as well as toxin production; in this case, the likelihood of CDI is elevated by up to 2-16 times.23 In addition, due to the recent emergence of hypervirulent strains, which are responsible for recurrent CDI and severe infections, the mortality rate of CDI patients is sharply increasing.24 Severe CDI in patients in LTCFs accounts for approximately 17-30% of all colitis, and the mortality rate of these patients was found to be 5-8%.22,25 Therefore, it is indicated that differential diagnosis should be performed for patients suspected of having colitis who were transferred from LTCFs. It has been indicated that risk factors including old age, history of antibiotics, accompanying serious vascular/cerebral nervous diseases, hypoalbuminemia, use of proton pump agents, and nursing period impact on the mortality rate of CDI patients in LTCFs.17,24,26 In the present study, all patients with a history of antibiotics were diagnosed with CDI; in the LTCFs group, 91% of patients were previously exposed to antibiotics, whilst 57% of patients in the local community group used antibiotics. In both groups, the cephalosporin class was the most frequently utilized, yet the statistical significance of this finding is limited given that (1) we included a small number of subjects in the study, and (2) it was not easy to confirm the types of agents used in the groups due to the retrospective nature of the study. We found that patients with decreased mental faculties showed significant results in univariate analysis regarding risk factors, indicating that exacerbated early conditions, as manifested by decreased mentality, are responsible for poor prognoses.
Consistent with other studies, we found that the average age of patients in LTCFs was >80 years, and that female patients outnumbered male patients. It is widely known that the diagnosis of colitis might be delayed in elderly patients because non-specific symptoms and infection signs can be present.16,27 Similarly, in patients from long-term facilities, their visit to our ER was delayed by 4 days from the occurrence of symptoms compared to patients in the local community group. This indicates that patients' conditions might worsen due to improper diagnosis and treatment in the early stage of disease. In fact, critical results might be caused (e.g., toxic mega-colon) if continuous anti-diarrheal agents/gastrointestinal motility suppressive agents are given for C. difficile or E. coli infection-related colitis, or if antibiotics are indiscriminately administrated for ischemic colitis and mild viral colitis, which may not require antibiotics.28,29 In blood tests, we found that hypoalbuminemia as well as increases in the numbers of WBCs were significantly different between the two groups; specifically, the average first albumin level in patients in the LTCFs group was 2.67 g/dL, which reflects poor nutrition and metabolic status, while WBCs were elevated more than 20×103/mm3, indicating a serious infection status compared to those of patients in the local community group. Reduced albumin level is often found in patients residing in LTCFs, and has been found to be associated with unfavorable prognoses; hence, nutritional support should not be underestimated for patients transferred from LTCFs.
The second most frequent form of colitis after CDI was found to be ischemic colitis in the LTCFs group, which accounted for 30% of total cases. In most patients of this group (i.e., patients transferred from LTCFs), hypertension was also present; in addition, multiple underlying diseases considered as risk factors for ischemic colitis, such as diabetes, cardiovascular disease, and arrhythmia were present and so differential diagnosis might be necessary. In a recent domestic study, early implementation of endoscopy and biopsy proved effective in the diagnosis of ischemic colitis as well as the identification of diseases in which similar clinical symptoms are observed.30 Therefore, observation of intestinal mucosa via colonoscopy or sigmoidoscopy early in the hospital stay is considered to be critical for treatment decisions and prognoses of patients who were transferred from LTCFs. In other countries, infection management guidelines of LTCFs recommend stool examinations in the early stage of colitis symptoms (e.g., diarrhea and vomiting) so that causative organisms can be assessed. Further, these guidelines stress the importance of comprehensive hygiene management as well as education for medical staff for the prevention of infectious colitis.13,16 In contrast, in South Korea, infection management and quality assessment of medical services is insufficient in LTCFs, and more attention as well as investigations are therefore warranted.
In the present study, we selected patients who represented relatively severe prognoses, and thus needed to be transferred to higher-tier hospitals, which led to a small sample size. Therefore, it is difficult to conclude that the results accurately reflect all cases of colitis in LTCFs. Furthermore, understanding of prognostic factors is limited due to differences in basal conditions between the different groups (i.e., patients from local communities vs. LTCFs). However, the results are still meaningful because this is the first study to investigate the clinical features as well as the essential factors for diagnosis by monitoring treatment prognoses and assessing the occurrence rate of different types of colitis in patients in LTCFs, which has never been studied before in South Korea.
Taken altogether, the occurrence rate of CDI was significantly higher in patients in LTCFs compared to those of the control group (i.e., local community patients), and patients were characterized with poor nutritional status and serious severity overall. Thus, indiscriminate use of anti-diarrheal agents should perhaps be avoided, while early implementations of stool examinations as well as supplementation of nutrition/fluids might be helpful if colitis symptoms are observed in such facilities. Further, the occurrence of complications and mortality rate could be improved by (1) early diagnosis through acquisition of specimens and observation of intestinal mucosa (2) implementation of treatment by tertiary hospitals after comprehensive review of medical history and medications, and (3) fast transfer to higher-tier hospitals if patients with decreased mentality and underlying diseases.
Notes
Financial support: None.
Conflict of interest: None.