Ustekinumab is effective in biological refractory Crohn’s disease patients–regardless of approval study selection criteria
Article information
Abstract
Background/Aims
Ustekinumab is effective in active Crohn’s disease. In a retrospective study, we assessed the clinical outcome in nonresponders to anti-tumor necrosis factor therapy, and/or conventional therapy and/or the α4β7-integrin inhibitor vedolizumab. As approval study populations do not always reflect the average “real world” patient cohort, we assessed weather patients who would not have qualified for approval studies show similar outcomes.
Methods
Forty-one patients with mild to severe active Crohn’s disease were treated with ustekinumab (intravenous 6 mg per kg/body weight) followed by subcutaneous ustekinumab (90 mg) at week 8. Depending on the clinical response maintenance therapy was chosen every 8 or 12 weeks. Clinical response was defined by Crohn’s Disease Activity Index (CDAI) decline, decline of stool frequency or clinical improvement. Inclusion criteria for approval studies were assessed.
Results
The 58.5% (24/41) showed clinical response to ustekinumab. The 58.3% of this group (14/24) achieved clinical remission. Clinical response correlated significantly with drop of stool frequency and improvement of CDAI score. The 39 out of 41 patients had no side effects and we observed no serious infections. About a third of our patients would not have met ustekinumab approval study criteria. However, patients who did not meet study criteria showed clinical improvement numerically in the same range compared to patients who would have qualified for approval studies.
Conclusions
Ustekinumab is effective, safe and well tolerated in a highly therapy refractory patient cohort. Even though a reasonable number of patients did not meet ustekinumab approval study criteria, approval study results seem to be representative to the overall patient cohort.
INTRODUCTION
Crohn’s disease (CD) is a chronic IBD mediated by different factors such as genetics, environment (e.g., food and smoking) and changes of gut microbiota–host interactions, altered by defects in the innate immune system of the gut [1,2]. Typically transmural lesions are observed and the whole gastrointestinal tract can be affected being characterized by periods of activity and remission [3,4].
The 0.3 to 20.1 cases per 100,000 persons in North America and 0.3 to 12.7 cases per 100,000 in European countries are affected by CD [5]. Especially in newly industrialized countries with Western lifestyle the incidence is rising in the past decade [6]. In these lines nutritional factors like high intake of polysatured fat or low levels of vitamin D might increase the risk of developing IBD [7,8]. Furthermore lifestyle dysbalances like disturbed sleep, stress and low physical activity are associated with a higher risk of CD [9,10], and vice versa, psychological issues like anxiety and quality of life are often affected by CD [11].
Current approved therapies for induction and maintenance of CD are corticosteroids, thiopurines, and biologicals including anti-TNF-antibodies, anti-integrin-antibodies like vedolizumab accomplished by the anti-interleukin 12 (IL-12) and IL-23 antibody ustekinumab [12]. Biologicals like anti-TNF agents (e.g., infliximab and adalimumab) are safe and effective but there is a significant rate of primary and secondary nonresponse affecting about 36% to 40% of patients [13-15]. Also the anti-integrin-antibody vedolizumab leads to sustained clinical remission in 27.7% of anti-TNF nonresponders at week 52 among patients who responded to vedolizumab induction at week 6 [16]. Despite this significant progress in treatment options for IBD, about 50% of CD patients need to be operated within 10 years of diagnosis and nearly 25% undergo a second operation within 5 years after first surgery [17]. Therefore, there is a tremendous medical need for development of further effective and safe drugs [18-21].
In the past years it came apparent, that an abnormal high IL-12 and IL-23 production might be one of the core inflammatory pathways activated in CD [22-24]. In these lines ustekinumab (STELARA®), a monoclonal antibody against the common p40 subunit of IL-12 and IL-23, was approved for the treatment of patients with moderate to severe active CD in 2016 (United States) and 2017 in Europe [25].
The approval was based on a phase IIb study (CERTIFI) and phase III study (UNITI), showing effectiveness of ustekinumab in induction and maintenance of remission in anti-TNF refractory and anti-TNF naive CD patients. However, clinical experience outside these studies is still limited [26,27]. Furthermore, in daily clinical care we often treat patients with biologicals like ustekinumab who would not have qualified for the above-mentioned approval studies. Those patients would not have met inclusion/exclusion criteria for various reasons. One common reason is, e.g., the CDAI range of therapy refractory patients which is often above or below the selection range of studies, despite clinical CD activity and need for therapy.
Therefore, the purpose of our retrospective analysis was to assess the clinical outcome in a selected, difficult to treat, tertiary care center patient group treated with ustekinumab, selected for therapy independent of phase II/III study inclusion criteria in a real-world setting. Finally, we evaluated potential markers of response including CRP, CDAI, and hemoglobin (Hb) values.
METHODS
We performed a retrospective analysis of patients with CD who have been treated with ustekinumab at the University Hospital Tübingen. The study was approved by the ethic committee of the University of Tübingen (approval No. 687/2012B01). Written informed consents were obtained. A group of 41 patients (>18 years) with mild to severe active CD (CDAI score, 93–775) who had either lost response or were intolerant to either conventional therapy (e.g., steroids, azathioprine, and methotrexate; n=32), vedolizumab (n=10) or TNF-α-antagonists (with or without vedolizumab therapy before; n=37) were treated with ustekinumab. Concomitant therapies with stable doses of azathioprine, methotrexate or steroids were permitted. Key inclusion criteria included diagnosis of CD ≥6 months before screening.
Therapy algorithm was intravenous treatment (6 mg/kg/body weight) at week 0 followed by subcutaneous ustekinumab (90 mg) at week 8. Depending on the clinical response patients were then either stopped or received maintenance therapy every 8 or 12 weeks (decision drawn by clinical observation, in terms of clinical response and patient well-being).
1. Data Collection
Baseline data were sex, age, weight, duration of disease, CRP - values, CDAI, prior medication, failure of previous treatment (any immunomodulatory drug, TNF-antagonist, failure criteria, primary/secondary nonresponse) (Tables 1, 2).
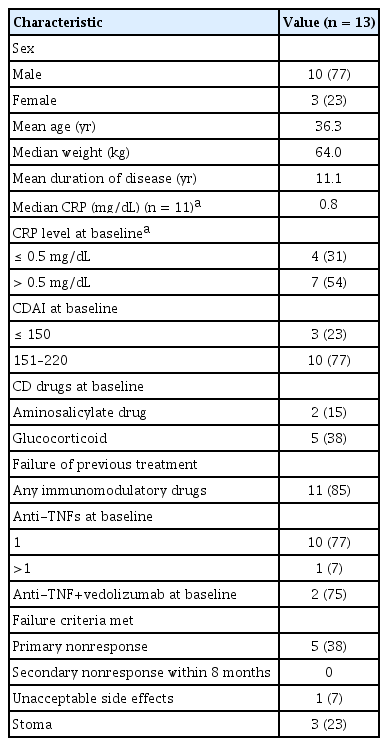
Baseline Characteristics of Patients with Remission (CDAI <150) and Mild Disease Activity (CDAI 151–220) before Application of Ustekinumab
Baseline Characteristics of Patients with Moderate to Severe Disease Activity (CDAI >221) before Application of Ustekinumab
Date of first ustekinumab application, concomitant medications, adverse events and the reason for discontinuation (intolerance, loss of response) were documented. Before starting therapy with ustekinumab Hb-values, CRP, CDAI and clinical assessment were documented.
2. Criteria for Clinical Response and Reason for Discontinuation of Ustekinumab
Clinical response was defined by either CDAI decline of more than 100 points, decline of stool frequency or clinical improvement as reported by patients (well-being) and physician’s global assessment. Clinical remission was defined as CDAI score of less than 150 points (for patients whose CDAI was above before therapy). Three patients were treated with ustekinumab even though they had a CDAI score <150 defined as remission. These patients were treated with ustekinumab because they lost response or became intolerant to their previous biological therapy (1 vedolizumab or 2 TNF-α-antagonists) and were early changed in a status of clinical remission, before exerting flare up (1/3 bridged with steroid use). In these patients, response was defined, e.g., as further clinical improvement (stool frequency and abdominal pain) or maintenance of previous remission. In all patients’ criteria for discontinuation were primary nonresponse (nonresponse 8 weeks after the first application), secondary nonresponse (initial response during maintenance therapy turned to loss of response) or intolerance.
3. Statistics
The presented graphs were generated using GraphPad Prism version 7 (GraphPad Software Inc., La Jolla, CA, USA). Statistical significance was assessed performing the paired t-test. P-values ≤0.05 were considered to be statistically significant.
RESULTS
1. Patient Characteristics
In total 41 patients with mild to severe CD activity were treated with ustekinumab from December 2016 to July 2018. The 38 out of 41 of the patients (92.7%) had been treated with immunomodulatory drugs before initiation of ustekinumab. The 10 out of 41 of the patients (24.4%) received at least one anti-TNF-antibody and vedolizumab before. The 28 out of 41 of the patients (68.3%) had been treated with 1 anti-TNF antibody and 10 with 2 or 3 anti-TNFs (24.4%) before start of ustekinumab (Tables 1, 2). The 15 out of 41 of the patients (36.6%) had concomitant therapy with glucocorticoids before application of ustekinumab. Only 3 out of 41 patients (7.3%) were biological naive (Tables 1, 2).
The 21 out of 41 of the patients (51.2%) were female. At the time-point of ustekinumab initiation median age of the patients was 35.9 years with a mean disease duration of 13.2 years. In 35 out of 41 patients (85.4%) CRP values were available before initiation of ustekinumab and the median serum level was 1.6 mg/dL (normal ≤0.5 mg/dL). All clinical characteristics of the patients are listed in Tables 1 and 2.
2. Clinical Response to Ustekinumab Therapy
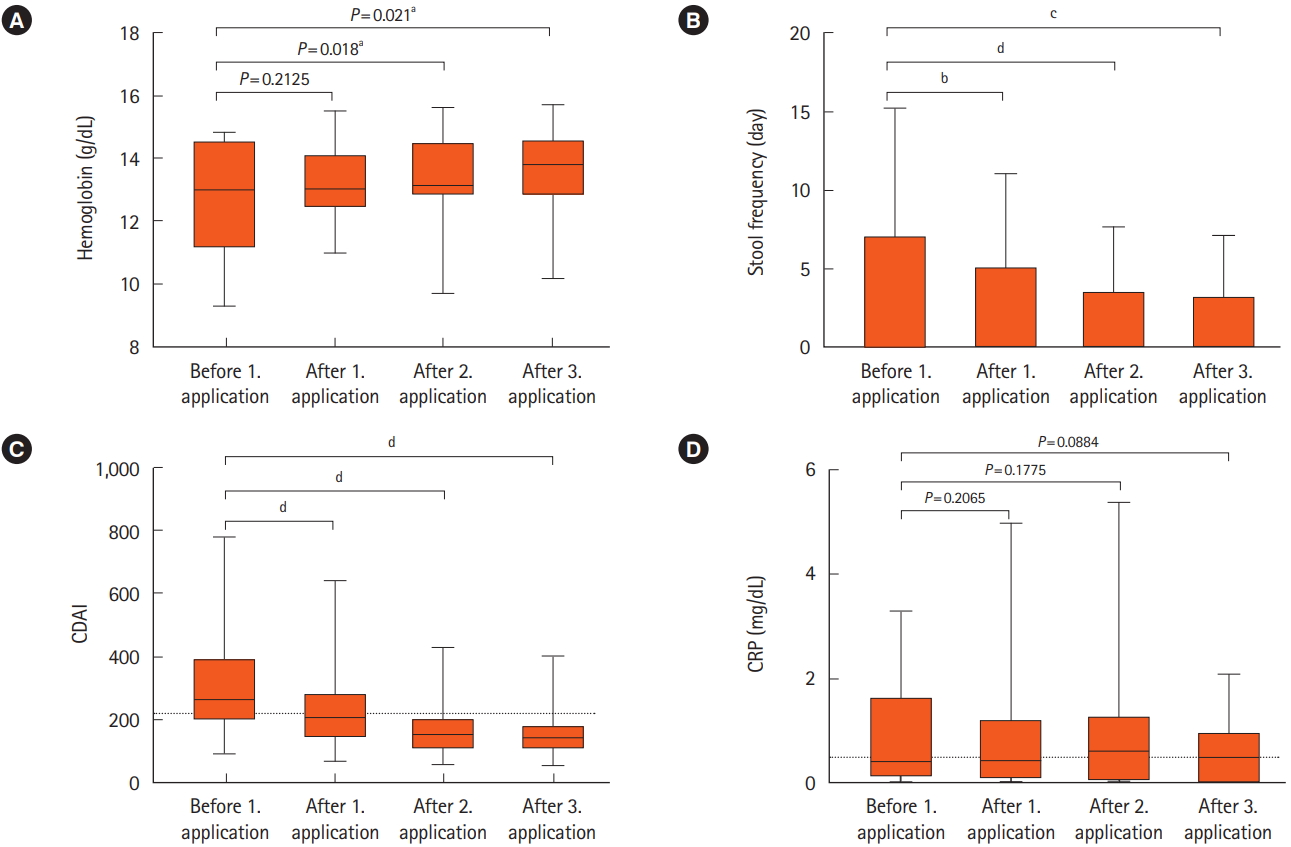
The observational period of the patients was 8 months after the first application of ustekinumab. The 14 out of 41 of the patients (34.1%) did not benefit from ustekinumab therapy (primary nonresponders) and in 3 cases initial response (7.3%) turned to a secondary nonresponse with increase of diarrhea frequency or/and abdominal pain (Fig. 1A).

Overall response and nonresponse towards ustekinumab. Shown are proportion of responders and nonresponders (A) and the characterization of primary responders (B). Clinical response was defined by either CDAI decline of more than 100 points, improvement as reported by patient’s well-being and physicians global assessment. Clinical remission was defined as CDAI score of less than 150 points. PR, primary response; PNR, primary nonresponse; SNR, secondary nonresponse (response that was not maintained).
Vice versa patients (24/41, 58.5%) responded to ustekinumab throughout the first 3 applications (primary responders) (Fig. 1A). Fourteen of these primary responders (58.3%; 34.1% of total population [14/41]) showed clinical remission (CDAI <150) and 10 (41.7%; 24.4% of total population [10/41]) developed clinical response (CDAI decline of more than 100 points, decline of stool frequency or clinical improvement defined by patients well-being and physicians observations) (Fig. 1B).
3. Development of Clinical Parameters in Primary Ustekinumab Responders
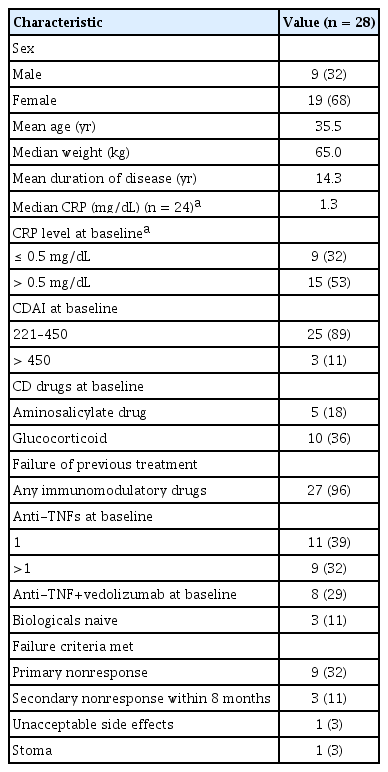
A significant increase of Hb-values could be observed after the first application of ustekinumab (n=21; P=0.018) (Fig. 2A). In 3 responders there were no Hb results available before starting therapy.
Follow-up of hemoglobin, stool frequency, CDAI, and CRP levels during treatment with ustekinumab. The graphics show the development of hemoglobin (A), stool frequency (B), CDAI (C), and CRP (D) during treatment with ustekinumab in the primary responder group from week 0 (before 1. application) to week 32 (after 3. application). Dotted line in panel C represents the threshold of flare-ups (CDAI score >220). Dotted line in panel D represents normal CRP value <0.5 mg/dL. Statistical relevance of the results was assessed performing the paired t-test. P≤0.05 was considered to be statistically significant. a P<0.05, b P<0.01, c P<0.001, d P<0.0001.
Also decline of stool frequency correlated positively with response after first (n=23; P=0.0016), second (n=23; P=0.0001) and third application (n=23; P=0.0002) (Fig. 2B). A significant effect was detected in CDAI decline after first (n=24; P=0.0001), second (n=24; P=0.0001) and third application (n=24; P= 0.0001), too (Fig. 2C).
After application of ustekinumab CRP levels were available in 19 responders after first, in 21 after the second and in 18 after the third application. However, there was no significant change in CRP levels after first (n=17; P=0.2114), second (n=16; P= 0.173) and third application (n=13; P=0.092) (Fig. 2D).
4. Ustekinumab Outcome by CRP-level (Normal Group vs. Elevated Group)
To further evaluate the prognostic value of baseline CRP levels, we investigated CRP-levels in 35 out of 41 of our patients, where CRP levels were available at baseline, before application of ustekinumab. Normal CRP levels are defined as ≤0.5 mg/dL in our clinical laboratory.
The 13 out of 35 had normal CRP-levels at baseline. The 69% of these patients had a primary response to ustekinumab, 23% showed primary nonresponse and 8% presented with secondary nonresponse during therapy with ustekinumab. In the elevated group (22/35), 41% of these patients showed a primary response, whereas 50% had a primary nonresponse and 9% developed a secondary nonresponse (Table 3). Therefore, patients with normal CRP -values had a higher probability of responding to ustekinumab in our patient cohort.
5. Clinical Outcome in Anti-TNF Refractory Patients (Anti-integrin Antibody Naive)
Of the 41 patients, 28 (68.3%) had been treated with at least one anti-TNF-antibody at baseline (Fig. 3A). In this group about half of the patients (12/28) were primary nonresponders to ustekinumab and 2 of the patients (7.1%) developed secondary nonresponse to ustekinumab (Fig. 3B). Vice versa (14/28) were primary responders. Characterizing these primary responders, we could observe that 75% (12/14) achieved clinical remission (CDAI <150) versus 2 patients with only a clinical response (Fig. 3C).
Response with respect to prior biological treatment. (A) Depicts the proportions of response with respect to prior biological treatment. Patients who had not been treated with a biological were defined as biological naive. (B) Focuses on patients with prior anti-TNF therapy. (C) Depicts response and remission of the primary responders. Clinical response was defined by either CDAI decline of more than 100 points, improvement as reported by patient’s well-being and physicians global assessment. Clinical remission was defined as CDAI score of less than 150 points. PR, primary response; PNR, primary nonresponse; SNR, secondary nonresponse (response that was not maintained).
6. Clinical Outcome of Anti-integrin/anti-TNF Pretreated Patients
Ten of the patients (10/41, 24.4%) had been treated with vedolizumab and at least one anti-TNF antagonist before initiation of ustekinumab. Seven of these patients (70%) showed a primary response, 2 nonresponse (20%) and 1 secondary nonresponse (10%) after 3 months (Fig. 4A). The 3 out of 7 of the responder (42.9%) in this group achieved clinical remission (Fig. 4B).
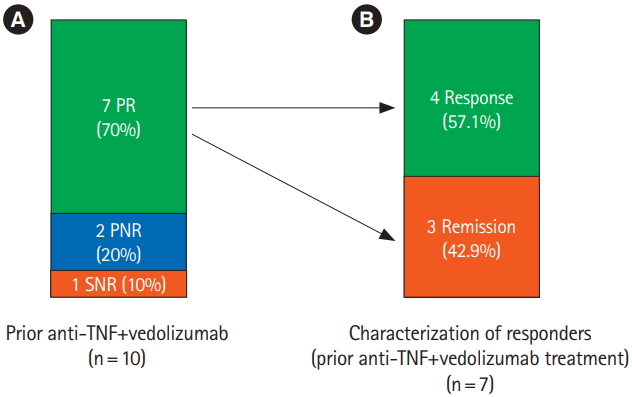
Response with respect to prior therapy with vedolizumab and anti-TNF. (A) Shows response rate with respect to prior therapy with vedolizumab and anti-TNF and (B) characterizes the responders of this group. Clinical response was defined by either CDAI decline of more than 100 points, improvement as reported by patient’s well-being and physicians global assessment. Clinical remission was defined as CDAI score of less than 150 points. PR, primary response; PNR, primary nonresponse; SNR, secondary nonresponse (response that was not maintained).
7. Clinical Response to Ustekinumab Treatment According to Primary or Secondary Loss of Response to Prior Anti-TNF-Therapy
The 17 of our patients (17/37, 45.9%) showed primary nonresponse to anti-TNF drugs. The 10 of these patients (10/17, 59%) showed primary response to ustekinumab, none of these patients developed secondary loss of response to ustekinumab.
The 20 of our patient cohort (20/37, 54.1%) had secondary nonresponse to prior anti-TNF-therapy. The 11 of these patients (11/20, 55%) showed primary response to ustekinumab and 3 out of 20 (15%) developed secondary nonresponse to ustekinumab (Table 4).
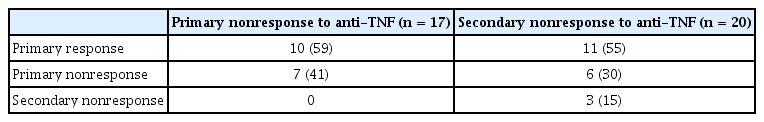
Primary versus Secondary Failure of anti-TNF–Relation to Type of Response to Ustekinumab Therapy (n=37)
Therefore, primary failure to anti-TNF-therapy is no marker to predict primary response to ustekinumab therapy (3/41 of our cohort [7.3%] were anti-TNF naive and in case of 1 patient there was no clear data about primary or secondary nonresponse).
8. Side Effects to Ustekinumab
During therapy only 2 patients (2/41, 4.9%) developed side effects after 3 and 5 months leading to therapy cessation. One patient was stopped because of developing arthralgia, dizziness and cephalgia and one patient because of skin blisters. The other patients (39/41) tolerated ustekinumab well. These data show an even better safety profile than the results of the approval study showing the percentages of patients with a serious adverse event being 9.9% and 12.1% with 90 mg of ustekinumab every 8 weeks, and every 12 weeks respectively [27]. Furthermore, we observed no related infections or deaths while in the approval study 2.3% in the group receiving ustekinumab every 8 weeks and 5.3% in the group receiving ustekinumab every 12 weeks and 2.3% in the placebo group developed serious infections [27].
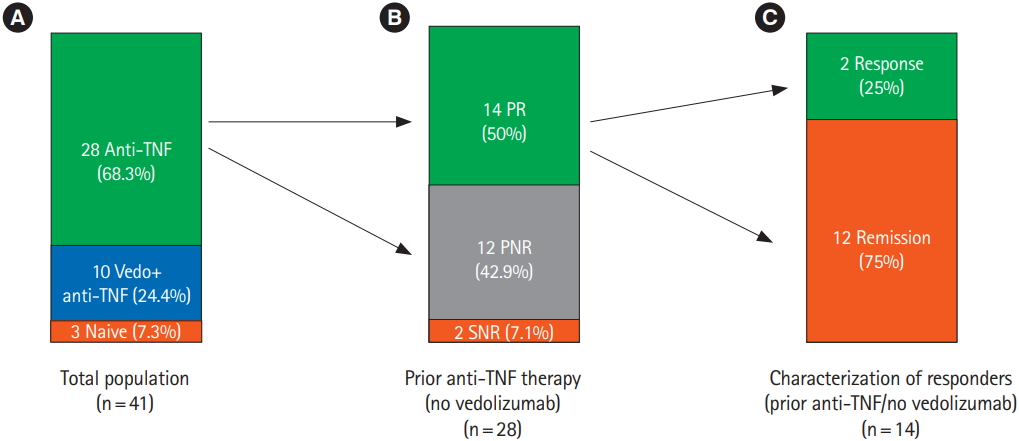
9. Patients Who Would Not Qualify for the Ustekinumab Approval Studies
As outlined in the introduction we were also interested in whether there is a difference in response to ustekinumab (in our patient cohort) between patients who would have qualified for the well-known phase II/III approval studies of ustekinumab and patients who would not have qualified for these studies. This question arises from the fact, that there seems to be a gap between patient collectives of IBD biological studies and real life IBD patients in daily clinical routine [28].
Sixteen patients of our cohort (16/41, 39%) would not have qualified for the phase II/III study inclusion criteria for different reasons–most common; CDAI >450 (n=3), 150–220 (n=10) or <150 (n=3) but clinical active disease defined, e.g., by abdominal pain. However, 11 of these patients (11/16, 68.7%) were responders to ustekinumab (Fig. 5A).
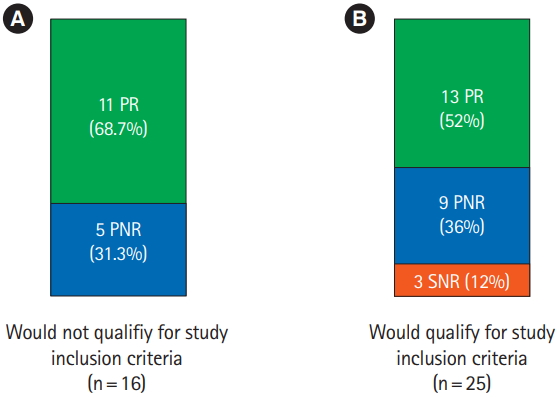
Comparison of patients qualifying for approval studies or who would not have qualified. Shown are the proportions of patients who would not (A) and would qualify (B) for the published ustekinumab approval studies and their response rates towards ustekinumab in our patient cohort. Clinical response was defined by either CDAI decline of more than 100 points, improvement as reported by patient’s well-being and physicians global assessment. Clinical remission was defined as CDAI score of less than 150 points. PR, primary response; PNR, primary nonresponse; SNR, secondary nonresponse.
10. Patients Who Would Have Qualified for Ustekinumab Approval Studies
Among our patient cohort (25/41, 61%) would have qualified for ustekinumab approval studies. In this group 13 (52%) were primary responders, 9 (36%) were primary nonresponders and 3 (12%) were secondary nonresponders (Fig. 5B). One of the approval studies achieved clinical remission rates of 46.1% and 40.3%, in the groups being treated with ustekinumab every 8 or 12 weeks [27].
DISCUSSION
In this study we retrospectively assessed the clinical outcome of CD patients’ refractory to conventional therapy (i.e., corticosteroids and immunosuppressants), anti-TNFs and/or vedolizumab receiving ustekinumab over a period of 8 months (3 applications). Our study provides further information for the efficacy and safety of ustekinumab in a real life, difficult to treat CD patient cohort. Overall, 92.7% of our patients failed at least one anti-TNF and 24.4% failed anti-TNF and vedolizumab before switch to ustekinumab. In this cohort 58.5% of the patients had a primary clinical response to ustekinumab therapy.
Clinical response was characterized by decrease of stool frequency, normalization of stool consistency, increased well-being with, e.g., less episodes of abdominal pain or improved fatigue and physicians evaluation. With this overall response rate our real life data (in terms of clinical improvement) are widely in line with the known approval study data of ustekinumab showing sustained remission rates of about 50% on doses of ustekinumab every 8 or 12 weeks [29]. The first real-life study about the efficacy of ustekinumab in a cohort of 38 severe anti-TNF resistant CD patients with a median follow-up of 7.9 months was performed by Kopylov et al. [30], showing initial clinical response in 73.7% of patients, even higher than those in our study population. One of the reasons for the difference might be the fact that our cohort consisted of extraordinarily biological resistant patients, for example ten of our patients were also refractory to vedolizumab. Kopylov et al. [30] did not treat the patients with vedolizumab before. A clinical response to ustekinumab of approximately 40% in real life practice was seen in 2 other studies in a cohort of 116 and 45 with a median follow-up of 10 and 12 months [29,31,32].
In our study there was no correlation between disease activity and the CRP-level after first, second and third application of ustekinumab. However, there are divergent data in the literature regarding CRP and its correlation to disease activity in CD. Some authors see it useful in the assessment and management of CD [33,34], others do not regard it as a reliable tool for monitoring CD activity.
Reasons for absence of CRP increase in CD patients might be previous application of antibiotics such as ciprofloxacin or metronidazole [35]. But also individual genetic factors may influence the CRP response and production. One aspect would be specific polymorphisms of the gene encoding CRP on the long arm of chromosome1 (1q23-24) leading to lower baseline of CRP production [36].
Only 2 of the patients (4.8%) in our cohort developed side effects to ustekinumab such as dizziness, skin blisters and arthralgia. No Infections were registered, underlining the favorable safety profile of ustekinumab in a real-life setting.
One of the main goals of our retrospective observation was to analyze the usefulness of common approval study selection criteria for biologicals in CD in real life patients. In clinical routine there is a diverse mixture of every kind of patients with different comorbidities and medical prehistory. However, in phase II/III studies of ustekinumab for example only patients with a CDAI-score between 220 and 450 were enrolled. In this case for example patients being treated with ustekinumab because of developing side effects towards anti-TNFs but having a clinical activity measured below CDAI <220 would not have been accepted in the studies [26,27]. Nevertheless, in clinical routine we often encounter this kind of patients and it is questionable if approval study selection is applicable to the average patients we treat in clinical routine. In our opinion our data suggest that approval study selection criteria generate clinical data which are transferable to the average CD patient regardless of fitting to study criteria. This conclusion is based on the fact that the clinical response rates in patients who would have qualified for approval studies (in our cohort) is not higher (even below) as they are in the patients who would not have qualified (Fig. 5). Therefore, this is a first advice that the criticism on approval study design in IBD [28] might not account for all biologicals.
Despite the small patient cohort and the follow-up of 8 months we believe that our study assessed valid and representative information for real-life use of ustekinumab. To sum up ustekinumab is a safe and effective drug for the treatment of patients refractory to conventional therapy, anti-TNFs and anti-integrins in CD, regardless of fitting to study selection criteria.
Notes
FINANCIAL SUPPORT
This work was supported by the Deutsche Forschungsgemeinschaft, Germany (Heisenberg Program).
CONFLICT OF INTEREST
J.W. received speakers honoray and/or consultant fees from Takeda, AbbVie, MSD, Ferring, Roche, Novartis, Janssen. T.K. received speakers honoray and/or consultant fees from Takeda, AbbVie, MSD, Novartis, Janssen. M.G. received speakers honoray and/or consultant fees from Takeda, AbbVie, MSD, Novartis, Janssen. Except for that, no potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION
Conceptualization: Saman S, Klag T, Wehkamp J. Methodology: Saman S, Klag T, Wehkamp J. Formal analysis: Saman S, Klag T, Wehkamp J, Wendler J, Goetz M. Funding acquisition: Wehkamp J, Malek NP. Project administration: Saman S, Klag T. Visualization: Saman S, Klag T, Wehkamp J, Wendler J, Malek NP. Writing - original draft: Saman S, Klag T, Wehkamp J. Writing - review and editing: all. Approval of final manuscript: all authors.

