Phenotypic characteristics of pediatric inflammatory bowel disease in Japan: results from a multicenter registry
Article information
Abstract
Background/Aims
There are few published registry studies from Asia on pediatric inflammatory bowel disease (IBD). Registry network data enable comparisons among ethnic groups. This study examined the characteristics of IBD in Japanese children and compared them with those in European children.
Methods
This was a cross-sectional multicenter registry study of newly diagnosed Japanese pediatric IBD patients. The Paris classification was used to categorize IBD features, and results were compared with published EUROKIDS data.
Results
A total of 265 pediatric IBD patients were initially registered, with 22 later excluded for having incomplete demographic data. For the analysis, 91 Crohn’s disease (CD), 146 ulcerative colitis (UC), and 6 IBD-unclassified cases were eligible. For age at diagnosis, 20.9% of CD, 21.9% of UC, and 83.3% of IBD-unclassified cases were diagnosed before age 10 years. For CD location, 18.7%, 13.2%, 64.8%, 47.3%, and 20.9% were classified as involving L1 (ileocecum), L2 (colon), L3 (ileocolon), L4a (esophagus/stomach/duodenum), and L4b (jejunum/proximal ileum), respectively. For UC extent, 76% were classified as E4 (pancolitis). For CD behavior, B1 (non-stricturing/non-penetrating), B2 (stricturing), B3 (penetrating), and B2B3 were seen in 83.5%, 11.0%, 3.3%, and 2.2%, respectively. A comparison between Japanese and European children showed less L2 involvement (13.2% vs. 27.3%, P< 0.01) but more L4a (47.3% vs. 29.6%, P< 0.01) and L3 (64.8% vs. 52.7%, P< 0.05) involvement in Japanese CD children. Pediatric perianal CD was more prevalent in Japanese children (34.1% vs. 9.7%, P< 0.01).
Conclusions
Upper gastrointestinal and perianal CD lesions are more common in Japanese children than in European children.
INTRODUCTION
Inflammatory bowel disease (IBD), which includes Crohn’s disease (CD), ulcerative colitis (UC), and IBD-unclassified (IBD-U), is a chronic inflammatory condition affecting the alimentary system. IBD can have physical, psychological, and social impacts on a patient’s life [1-6]. These conditions affect millions of people globally and cause debilitating symptoms that impair function and quality of life [7-9]. The number of people with IBD is increasing worldwide, including in Asia [10-14], and up to a quarter of patients with IBD experience disease onset during childhood [15]. The characteristics of pediatric IBD have been described in studies from single large institutions or studies based on nationwide and regional registries [11,14,16-26]; however, few studies were from Asia. Additionally, although young children with IBD have a higher incidence of isolated extensive colonic disease [27], few studies have investigated the phenotypic characteristics of Asian children with IBD in the multicenter prospective registry setting. To fill this gap in knowledge, the current study used the Japanese Pediatric Inflammatory Bowel Disease Registry (JPIBD-R) network and examined the cross-sectional registry of newly diagnosed pediatric IBD patients. The study characterized the features of IBD using the Paris classification [28] and compared the results with published European registry (EUROKIDS) network data [18,21].
METHODS
1. Ethical Considerations
The study was approved by the institutional review boards at all participating institutions. Informed consent was obtained from the parents of young children, and signed youth consent was obtained from patients enrolled with the JPIBD-R, where appropriate.
2. JPIBD-R
The JPIBD-R network was formed in 2012 by 15 institutions in Japan. The JPIBD-R is a cross-sectional registry of newly diagnosed Japanese pediatric IBD patients. The JPIBD-R started enrolling patients in November 2012. As of December 2015, 20 institutions are actively involved in the network, with 265 patients registered electronically. Most participating institutions are tertiary children’s hospitals or university hospitals capable of diagnosing and managing pediatric IBD using imaging studies or pathology. Although 4 of the 20 institutions are community hospitals, their pediatricians are active members of the Japanese Society for Pediatric IBD.
3. Patient Eligibility
Patients who were 17 years old or younger at the time of diagnosis were eligible for enrollment. The Porto criteria was applied for the diagnosis of IBD, including UC, CD, and indeterminate colitis [29]. After the revision of the Porto criteria in 2014 [30], the term “indeterminate colitis” was replaced with IBD-U. This is because the Paris classification, which we used to characterize the phenotypic features of our patients, uses the term “IBD-U” instead of “indeterminate colitis.” The participating institutions were encouraged to apply the revised Porto criteria for the diagnosis of IBD.
Besides the assessments of clinical signs and symptoms, complete examinations for the diagnosis of IBD included a colonoscopy with ileal intubation, an upper gastrointestinal (GI) endoscopy, and small-bowel imaging. In patients with definite UC, upper GI endoscopy and small-bowel imaging may not be performed. For small-bowel imaging, small-bowel follow-through, magnetic resonance enterography, wireless capsule endoscopy, computed tomography, ultrasonography, and balloon-assisted enteroscopy were used to evaluate small-bowel lesions. Multiple biopsies from all segments of the GI tract were prepared for histologic evaluation.
One exclusion criterion was incomplete demographic data. Moreover, patients who did not undergo an upper GI endoscopy or total colonoscopy, or did not have at least one small-bowel imaging finding for the diagnosis of CD and IBD-U were excluded. Those without ileal intubation were included if other small-bowel imaging examinations were complete. Patients who did not undergo a total colonoscopy for the diagnosis of UC were excluded. Patients who did not undergo an upper GI endoscopy and ileal intubation, or did not have small-bowel imaging data were included if the diagnosing physician had based the diagnosis of UC on clinical, total colonoscopy, and histologic findings.
Demographic data included date of birth, sex, body weight, height, parental height, date of disease onset, symptoms at onset, diagnosis of IBD, date of diagnosis, family history (first-degree relatives with IBD), complications, and disease location and behavior according to the Paris classification for CD, as well as the extent and severity of the disease according to the Paris classification for UC.
4. Paris Classification
The Paris classification was published in 2010 as an evidence-based pediatric modification of the Montreal classification [28]. In the current study, the Paris classification was used to classify IBD, age at diagnosis and delayed growth to classify all IBD, disease location and behavior to classify CD, and disease extent and severity to classify UC. A1a was defined as IBD diagnosed before the age of 10 years, and A1b was defined as IBD diagnosed after the age of 10 years but before the age of 17 years. A2 was defined as IBD diagnosed after the age of 17 years but before the age of 40 years. We further categorized patients whose disease was diagnosed before the age of 6 years as having very early onset (VEO)-IBD.
For CD location, the results of appropriate imaging studies, including upper GI endoscopy, colonoscopy with or without ileal intubation, and at least one small-bowel imaging examination, were used. The location was categorized as L1 (involving one-third of the distal ileum only with limited or no cecal disease), L2 (colonic involvement only), L3 (involvement of both the terminal ileum and colon), L4a (esophagogastroduodenal disease), and L4b (involvement of the jejunum and/or proximal two-third of the ileum). As previously reported [18], L4a (upper GI lesion) was defined as the presence of ulcerations, erosions/aphthae, cobblestones, and/or stenosis. According to endoscopic findings, the extent of UC was categorized as E1 (proctitis only), E2 (left-sided colitis, distal to the splenic flexure), E3 (extensive colitis, distal to the hepatic flexure), and E4 (pancolitis proximal to the hepatic flexure).
Specific findings on rectal sparing, backwash ileitis, and cecal patch were not compiled in this registry network.
CD behavior was categorized according to the presence of strictures, intra-abdominal fistulas, and/or intra-abdominal abscesses into B1 (non-stricturing, non-penetrating disease), B2 (stricturing disease), B3 (penetrating disease excluding isolated perianal or rectovaginal fistulas), and B2B3 (presence of both B2 and B3 phenotypes in the same patient). In addition, p (perianal disease modifier) was defined as the presence of a fistula, anal canal ulcer, or abscess. Isolated skin tags, fissures, or hemorrhoids were not considered perianal disease.
UC severity was defined as a pediatric UC activity index score of ≥ 65, and was categorized as S0 (never severe) or S1 (ever severe) [31].
Growth delay at diagnosis, G1, was defined as the difference between the observed height z-score and the predicted z-score using the mid-parental height formula of > 2.0, or the difference between the observed height z-score and the pre-illness height z-score of > 1.0. Normal growth at diagnosis, G0, was assigned to patients who did not meet the above criteria.
Implementation of the revised Porto criteria and the Paris classification was recommended to the participating institutions at annual face-to-face meetings and in bimonthly newsletters.
5. Comparison of Disease by Age Group
Disease diagnosis, family history, location and CD profile, and UC extent and severity in the JPIBD-R network were compared among 3 age groups, as follows: diagnosis before the age of 6 years (VEO-IBD), diagnosis between the ages of 6 and 9 years, and diagnosis between the ages of 10 and 17 years.
6. Comparison of JPIBD-R with EUROKIDS
The results of the JPIBD-R were compared with those of the EUROKIDS registry published in 2013 [18,21]. Age at diagnosis, disease location and disease behavior for CD, and disease extent for UC were compared.
7. Statistics
Descriptive data were calculated as percentages for discrete findings. Age at diagnosis was presented as mean ± standard deviation. Duration between the disease onset and the diagnosis was presented as median and interquartile range. To test differences between more than 2 categories of disease location or disease behavior, the chi-square test or Fisher exact test was used, where appropriate. Two-sample t-tests were used to compare 2 continuous variables.
For disease behavior of CD, and growth of CD and UC, data were expressed as the median and interquartile range for their skewed distribution. The duration between the disease onset and the diagnosis for these variables were compared using the Mann–Whitney U test.
To identify the variables of perianal modifiers, logistic regression analysis was performed.
Statistical significance was defined as a two-tailed P-value of < 0.05 using SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL, USA) and EZR (Jichi Medical University, Saitama, Japan).
RESULTS
1. Patients’ Baseline Demographic Variables
Between November 2012 and December 2015, 265 patients from 20 independent institutions (16 tertiary children’s hospitals or university hospitals and 4 community hospitals with pediatric wards) were registered using the web-based registration system of the JPIBD-R. Among the 265 patients, 22 were excluded for incomplete demographic data. Among the remaining 243 patients, 91 were diagnosed with CD, 146 with UC, and 6 with IBD-U (Fig. 1). The baseline demographic features of the patients are summarized in Table 1.
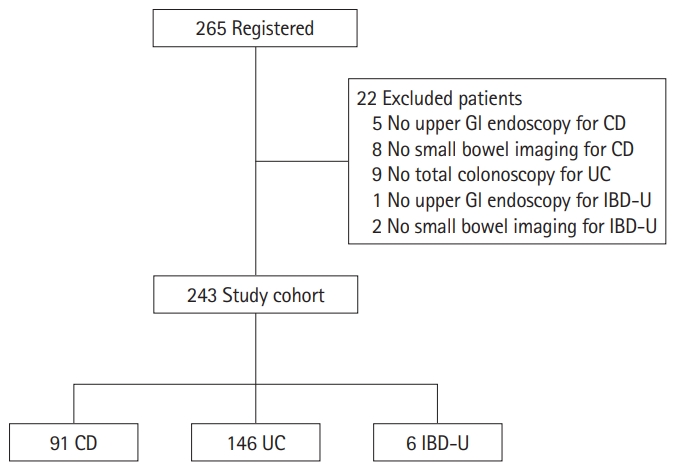
Study flowchart. Flowchart showing patient registration and inclusion/exclusion from analysis. GI, gastrointestinal; CD, Crohn’s disease; UC, ulcerative colitis; IBD, inflammatory bowel disease; IBD-U, IBD-unclassified.
2. Extraintestinal Manifestations
The extraintestinal manifestations or comorbidities at CD diagnosis included arthritis (n = 3), primary sclerosing cholangitis (n = 2), erythema nodosum (n = 1), splenic abscess (n = 1), vitiligo vulgaris (n = 1), scleritis (n = 1), and Weber–Christian disease (n = 1). For UC, primary sclerosing cholangitis (n = 1) and pyoderma gangrenosum (n = 1) were noted as extraintestinal manifestation.
3. Disease Location and Extent
The location and extent of the disease at the time of diagnosis for both CD and UC, based on the Paris classification [28], are shown in Table 2. Children with VEO-CD showed less L3 involvement than older children with CD. In UC, children with VEO-UC showed more extensive disease than older children; however, the difference was not statistically significant.
4. Disease Behavior in CD
The disease behavior of CD is shown in Table 1. Among the 19 children under the age of 10 years, 1 patient (5.3%) was categorized as B2B3 and the rest (94.7%) as B1. Among those between 10 and 17 years of age, 13.9% were categorized as B2, 4.2% as B3, and 1.4% as B2B3. The duration between the disease onset and the diagnosis was longer in B2, B3, or B2B3 (194 days [105.5–312.5]) compared to B1 (119 days [58.0–274.5]) (P= 0.183).
For perianal lesions, 31 of the 91 cases of CD patients (34.1%) were defined as having perianal disease modifiers (Table 2). The duration between the disease onset and diagnosis was significantly shorter in p (+) (92 days [55.0–198.5]) compared to p (–) (155 days [115.5–810.5]) (P< 0.01).
5. Disease Severity in UC
The disease severity at the time of diagnosis was evaluated in 98.6% of the 146 UC patients (144 of 146 cases). Among these, S1 (defined as a pediatric UC activity index score of ≥ 65) was noted in 21.5% (31 of 144 cases). Only 1 of 16 patients (6.3%) in the 6–9 years age range and none of those younger than 6 years were defined as having S1; however, 30 of 112 patients (26.8%) in the 10–17 years age range were defined as having S1 (P< 0.01).
6. Growth
At the time of diagnosis, 79 of 91 total CD cases were evaluated for impaired or delayed growth, and it was observed in 7.6% of cases (6/79). The duration between disease onset and diagnoses was equivalent between categories G1 (169.5 days [52.3–661.0]) and G0 (110.5 days [59.8–260.3]) (P= 0.701). In UC cases, 128 patients of the 146 were evaluated at the time of diagnosis, and delayed or impaired growth was observed in 7.8% of cases (10/128). The duration between the disease onset and the diagnosis was longer in category G1 (144 days [63.0–226.0]) compared to G0 (62.5 days [30.3–170.5]) (P= 0.183).
7. Comparison between Japanese and European Children with IBD
The results of comparisons between JPIBD-R and EUROKIDS for disease location and behavior of CD are summarized in Table 3. Age at the time of diagnosis was similar between JPIBD-R and EUROKIDS for both CD and UC (Fig. 2). There was significantly less L2 involvement (P< 0.01) but more L3 (P< 0.05) and L4a (P< 0.01) involvement in JPIBD-R than in EUROKIDS. There were no significant differences in disease behaviors (B1, B2, B3, and B2B3) except that perianal disease modifiers were significantly prevalent in JPIBD-R (P< 0.001). UC extent was similar between JPIBD-R and EUROKIDS (Table 3).

Age at diagnosis of inflammatory bowel disease (IBD) according to Paris classification criteria. A1a, IBD diagnosed before age 10 years; A1b, IBD diagnosed at age ≥10 years but before age 17 years; A2, IBD diagnosed at age ≥17 years but before age 40 years; CD, Crohn’s disease; UC, ulcerative colitis; JPIBD-R, Japan Pediatric Inflammatory Bowel Disease Registry; EUROKIDS, EUROKIDS registry.
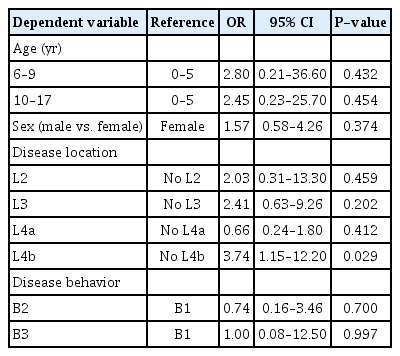
8. Factors Associated with Perianal Disease Modifiers
Logistic regression analysis was performed by factoring perianal disease modifiers as a dependent variable, whereas age, sex, disease location, and disease behavior were taken as independent variables. Table 4 shows the adjusted odds ratios, 95% confidence intervals, and P-values. Perianal disease was significantly more prevalent in children with L4b than in those without L4b (P< 0.05). The estimated power of association between perianal lesions and L4b was 67%.
DISCUSSION
To our knowledge, this is the largest multicenter cross-sectional registry study on IBD phenotypes in Asian children. Applying uniform classification criteria enabled us to conduct a cross-ethnic comparison of IBD between Asian and European cohorts in a prospective setting. We found a higher incidence of upper GI (L4a), ileocolonic (L3), and perianal involvement in Japanese children with CD than in European children [18]. We also found less colonic involvement (L2) in Japanese children.
In the EUROKIDS studies [18,21], up to 14% of UC cases and 52% of CD cases were excluded from the analyses because of an incomplete diagnosis or missing data. In contrast, only 4% of UC cases and 9% of CD cases were excluded from analysis in the JPIBD-R. This may be because, in this single-nation registry setting, there were fewer institutions from which to compile data than in the pan-European setting [18,21]. Additionally, the availability of imaging modalities at most institutions in Japan may have strengthened our findings.
For disease location, children with CD in the JPIBD-R showed less colonic involvement but more upper GI, ileocolonic, and perianal involvement than European children [18,21]. Younger CD patients show more colonic involvement than older patients; however, the age distributions in JPIBD-R and EUROKIDS were similar. Children in the JPIBD-R showed a higher prevalence of L4a (upper GI disease) than those in EUROKIDS; however, a subgroup analysis of EUROKIDS revealed no significant difference in L4a by ethnicity. According to a EUROKIDS study [18], L4b was more prevalent in Asians; however, in the JPIBD-R population, L4b seemed less prevalent.
Interestingly, children with CD in the JPIBD-R had a higher incidence of perianal disease than European children [18], and logistic regression analysis showed that perianal disease was more prevalent in those with L4b. The incidence of perianal CD at diagnosis in children in North America and Europe ranged between 3% and 15% [16,18,19,22,24]. The incidence rate based on the JPIBD-R was more than three times higher than that in EUROKIDS [18]. Large data from a prospective observational cohort, the ImproveCareNow Network, revealed a racial difference in the incidence of perianal disease [32]. Blacks had significantly higher incidence of perianal disease than whites (26% vs. 20%). The incidence rate of perianal disease in this Asian cohort was 24%. However, the patients included those who had developed perianal disease during the follow-up, and the incidence at diagnosis remained < 10% in all races including Asian. Contrarily, a prospective clinical comparison of adults with CD in Australia and Hong Kong reported a higher incidence of perianal disease in Hong Kong (15.8% vs. 35.4%) [33]. Similarly, a population-based study involving 9 countries in the Asia-Pacific region reported a higher incidence of perianal disease in Asia than in Australia (19% vs. 2%), with the incidence being the highest in mainland China compared with the rest of Asia (33%–66% vs. 10%–16%) [14]. A small single-institution retrospective review of 30 South Korean children with CD also revealed a higher prevalence of perianal disease (33.3%) [20]. It is possible that there may be a genetic component that predisposes a person to perianal lesions, and cross-ethnic genetic comparisons should be performed.
In UC, the extent of disease at diagnosis was similar between JPIBD-R and EUROKIDS. However, EUROKIDS reported the incidence of rectal sparing, backwash ileitis, and upper GI involvement, whereas our registry network analyses failed to itemize these features. For the severity of UC, although children with VEO-UC seemed to be severe and refractory to medication compared with the older population [33], none of the VEO-UC cases were considered severe UC (pediatric UC activity index score of ≥ 65) at diagnosis.
This study had some limitations. First, JPIBD-R is not a population-based cohort registry but a cross-sectional registry. This means that there could be selection bias. However, because of the shortage of pediatric gastroenterologists in Japan, the available ones need to manage pediatric IBD cases with wide-ranging severities. Therefore, the data on the phenotypes of pediatric IBD would reflect population-based data. Second, there were relatively small numbers of patients in each subgroup, which may have limited the statistical analyses. Finally, the lack of a central evaluation system for endoscopic and histologic findings in this registry may have allowed for inter-observer variation. However, we considered the reliability of diagnosis to be relatively high because the participating institutions were able to perform the required imaging studies and were able to adequately interpret the histopathology of mucosal biopsies.
In conclusion, a thorough systematic evaluation of IBD in children by using a prospective multicenter registry in Japan revealed a different disease distribution between Japanese and European children with CD. Less colonic, but more upper GI and perianal, involvement was observed in the Japanese pediatric CD population. The results suggest that environmental and genetic factors may contribute to the phenotype of CD. Future studies with a larger number of pediatric patients and with a longer follow-up are needed to strengthen the current findings. We believe that data from genotype–phenotype studies may reveal different IBD distributions among ethnic populations worldwide. Attention should be paid to the differences among ethnic groups in future genotype–phenotype studies with cross-cultural participation. Data from genotype–phenotype studies will provide support for better IBD management in therapeutic settings.
Notes
FINANCIAL SUPPORT
This work was supported in part by a Grant-in-Aid for the National Center for Child Health and Development, and by a Health and Labour Science Research Grant for Research on Intractable Diseases from the Ministry of Health, Labour and Welfare of Japan.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION
Conceptualization: Arai K, Shimizu T, Shimizu H, Suzuki Y, Fujiwara T. Data curation: Arai K, Hirano Y. Formal analysis: Hirano Y, Fujiwara T. Funding acquisition: Arai K, Suzuki Y. Methodology: Arai K, Kakuta F, Shimizu T, Aomatsu T, Inoue M, Saito T, Shimizu H, Hirano Y, Fujiwara T. Project administration: Arai K, Hirano Y. Visualization: Hirano Y. Writing – original draft: Arai K. Writing – review and editing: Arai K, Kunisaki R, Hirano Y. Approval of final manuscript: all authors.
Acknowledgements
The authors thank Dr. Julian Tang from the Department of Education for Clinical Research, National Center for Child Health and Development, Japan, for reviewing this manuscript. The authors also thank Dr. Eisuke Inoue, Division of Biostatistics, Center for Clinical Research and Development, National Center for Child Health and Development, Japan, for a critical review of the statistical analyses.