|
 |
- Search
| Intest Res > Volume 20(1); 2022 > Article |
|
Abstract
Background/Aims
Methods
Results
ADDITIONAL INFORMATION
Funding Source
The authors received no financial support for the research, authorship, and/or publication of this article.
Author Contribution
Conceptualization: Sakurai K, Furukawa S, Katsurada T, Otagiri S, Yamanashi K, Onishi R, Yagisawa K, Nishimura H, Ito T, Maemoto A, Sakamoto N. Data curation: Sakurai K. Formal analysis: Sakurai K, Katsurada T, Otagiri S. Investigation: Sakurai K, Otagiri S. Methodology: Sakurai K, Furukawa S, Katsurada T, Otagiri S. Project administration: Sakurai K, Furukawa S, Otagiri S. Resources: Sakurai K, Katsurada T, Otagiri S. Software: Sakurai K, Otagiri S. Supervision: all authors. Validation: Sakurai K, Katsurada T, Otagiri S. Visualization: Sakurai K, Otagirip S. Writing - original draft: Sakuraip K. Writing - review & editing: Sakurai K, Katsurada T, Otagiri S, Nagashima K, Onishi R. Approval of final manuscript: all authors.
Supplementary Material
Fig. 1.
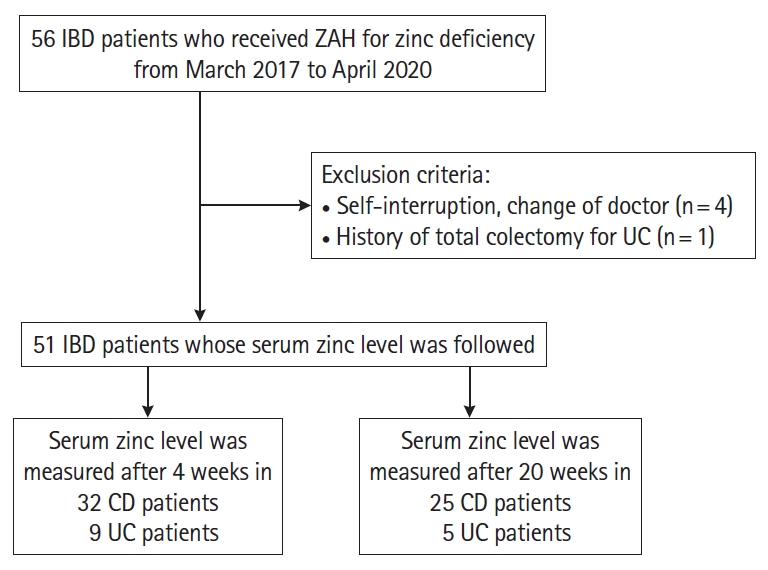
Fig. 2.

Fig. 3.
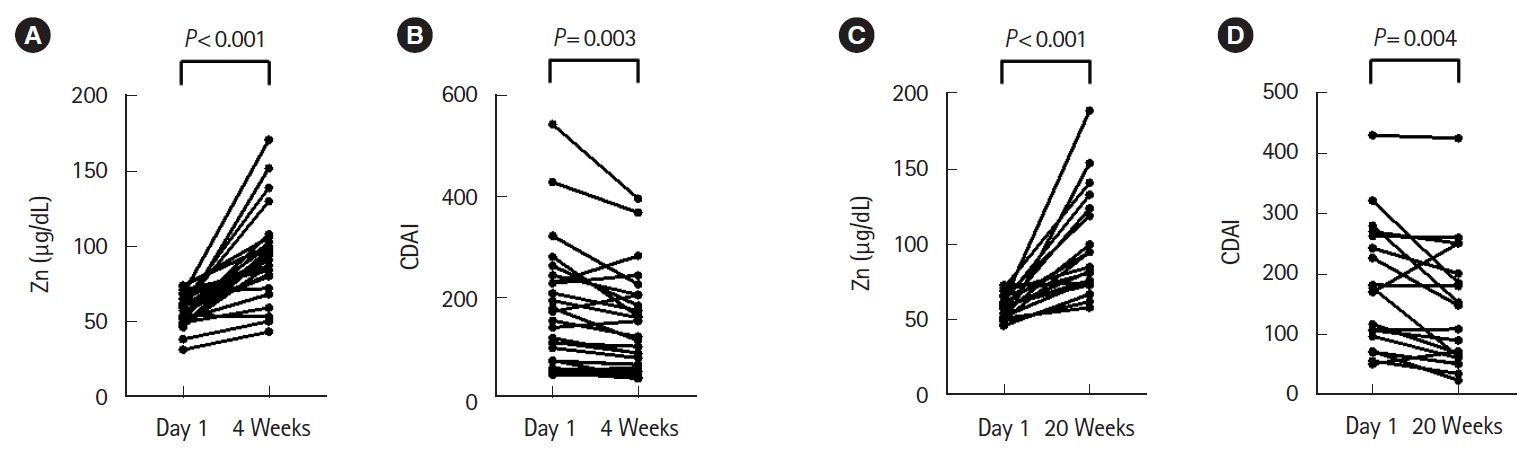
Fig. 4.
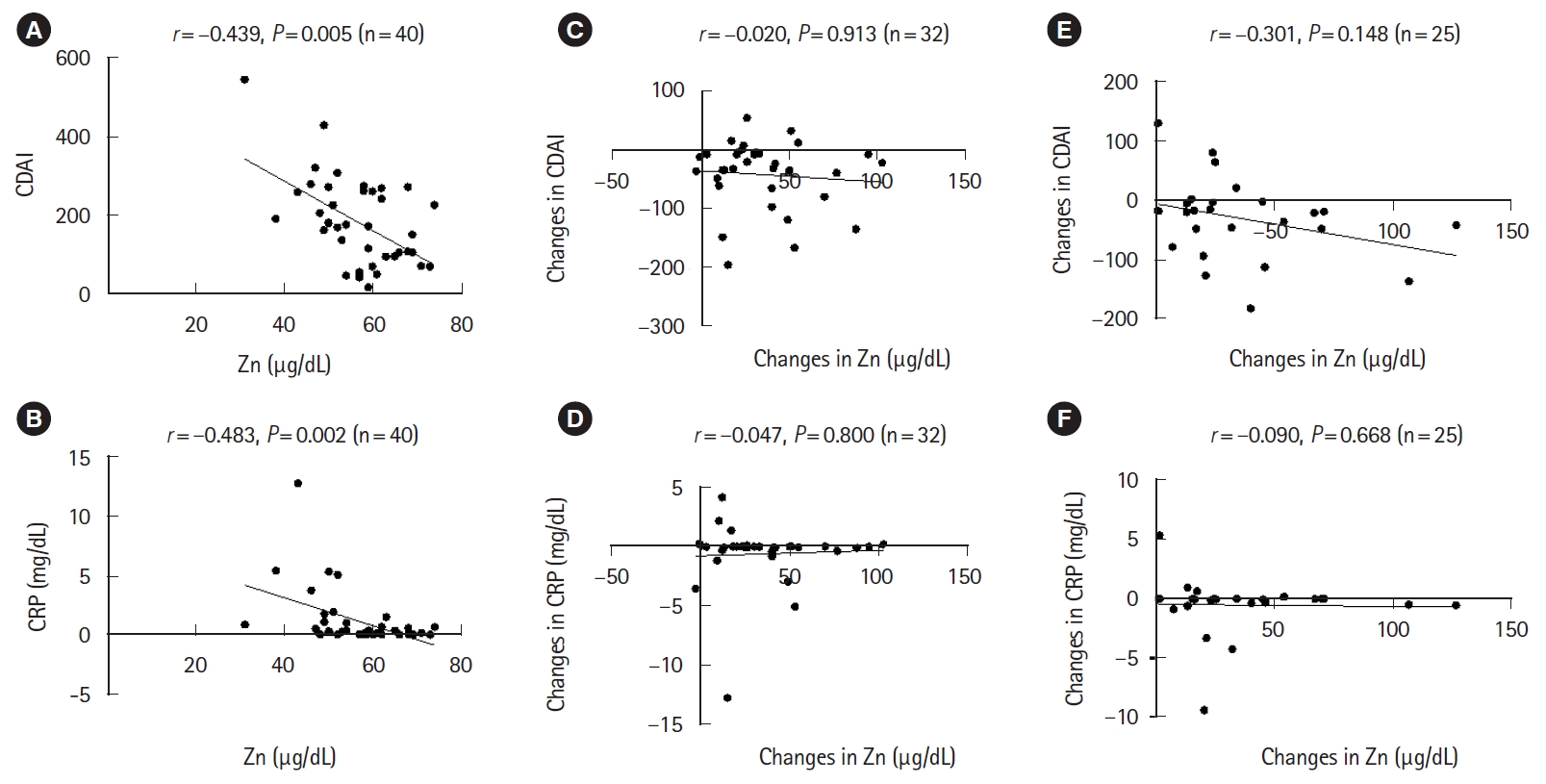
Fig. 5.
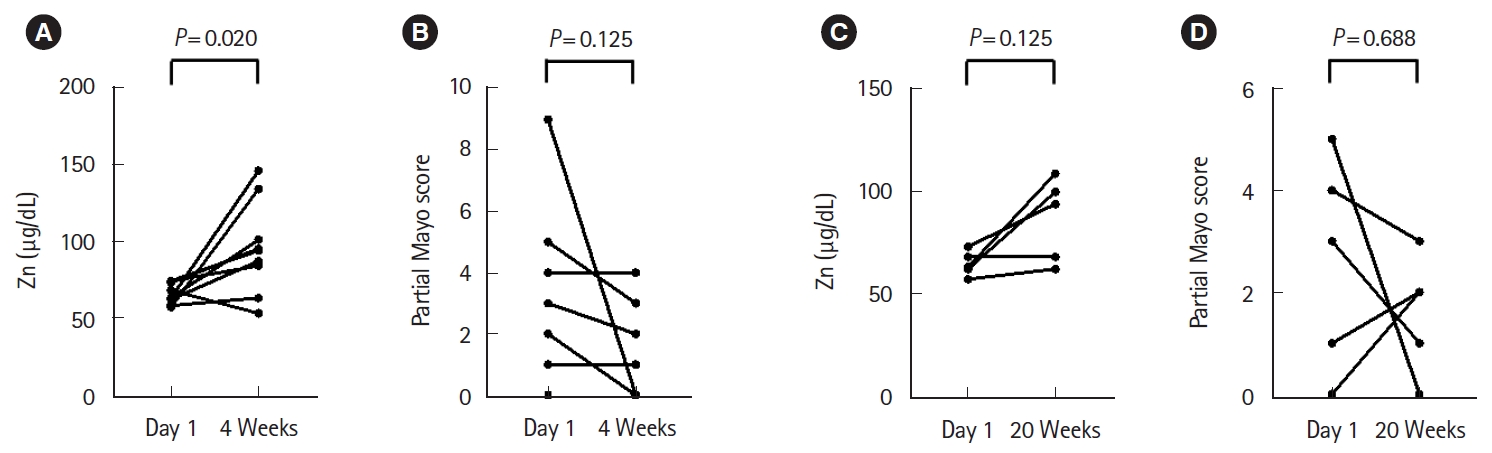
Table 1.
Values are presented as median (range) or number (%). CD, Crohn's disease; UC, ulcerative colitis; CDAI, Crohn’s Disease Activity Index; pMayo, partial Mayo score; ZAH, zinc acetate hydrate; 5-ASA, 5-aminosalicylic acid; SASP, salazosulfapyridine; TNF, tumor necrosis factor; IL, interleukin; JAK, Janus kinase.
Table 2.
Values are presented as median (range) or number (%).
CD, Crohn's disease; ZAH, zinc acetate hydrate; CDAI, Crohn’s Disease Activity Index; CRP, C-reactive protein; 5-ASA, 5-aminosalicylic acid; SASP, salazosulfapyridine; TNF, tumor necrosis factor; IL, interleukin; NS, not significant.
P-values were calculated using the chi-square test for categorical variables and Mann Whitney test for continuous variables.
Table 3.
Values are presented as median (range) or number (%).
CD, Crohn's disease; ZAH, zinc acetate hydrate; CDAI, Crohn’s Disease Activity Index; CRP, C-reactive protein; 5-ASA, 5-aminosalicylic acid; SASP, salazosulfapyridine; TNF, tumor necrosis factor; IL, interleukin; NS, not significant.
P-values were calculated using the chi-square test for categorical variables and Mann Whitney test for continuous variables.