Assessing quality of magnetic resonance enterography and its impact on disease assessment of ileal Crohn’s disease
Article information
Abstract
Background/Aims
Assessment of quality of magnetic resonance enterography (MRE) in small bowel Crohn’s disease (CD) activity evaluation has received little attention. We assessed the impact of bowel distention and motion artifact on MRE activity indices in ileal CD.
Methods
A cohort of patients who underwent contemporaneous MRE and colonoscopy for ileal CD assessment between 2014 and 2021 at 2 centers were audited. An abdominal radiologist blinded to clinical data reviewed each MRE, graded bowel distention and motion artifact upon a pre-specified 3-point scale and calculated the original magnetic resonance index of activity (MaRIA) and simplified MaRIA (sMaRIA), London index and CD MRE index (CDMI). Ileal endoscopic activity was graded via the Simplified Endoscopy Score for CD (SES-CD). The performance of MRE indices in discriminating active disease (SES-CD ≥3) stratified by MRE quality was measured by receiver operator characteristic analyses.
Results
One hundred and thirty-seven patients had MRE and colonoscopy within a median of 16 days (range, 0–30 days) with 63 (46%) exhibiting active disease (SES-CD ≥3). Forty-four MREs (32%) were deemed low quality due to motion artifact and/or moderate to poor distention. Low-quality MREs demonstrated reduced discriminative performance between ileal SES-CD ≥3 and MRE indices (MaRIA 0.838 vs. 0.634, sMaRIA 0.834 vs. 0.527, CDMI 0.850 vs. 0.595, London 0.748 vs. 0.511, P<0.05 for all). Individually the presence of any motion artifact markedly impacted the discriminative performance (e.g., sMaRIA area under the curve 0.544 vs. 0.814, P<0.05).
Conclusions
Image quality parameters can significantly impact MRE disease activity interpretation. Quality metrics should be reported, enabling cautious interpretation in lower-quality studies.
INTRODUCTION
Crohn’s disease (CD) is a chronic immune-mediated condition that can manifest anywhere throughout the entire gastrointestinal tract and can be associated with a variety of extraintestinal manifestations [1]. European population studies have demonstrated an incidence of 322 per 100,000 persons. Most commonly CD involves the terminal ileum with complications including stricturing and/or penetrating complications such as fistula, abscess and phlegmon formation with ensuing risk of bowel perforation [2,3]. With advances in therapeutics and early, aggressive initiation of therapy, the risk of developing complications from long-standing disease can be mitigated [4].
Objective disease activity assessment is integral to therapeutic decision-making. Recent STRIDE 2 expert consensus guidelines in inflammatory bowel disease (IBD) advocate for frequent objective activity assessments with the target of achieving remission [5]. In patients with small bowel CD, the gold standard of disease activity assessment remains thorough endoscopic evaluation however endoscopy is subject to several challenges [6]. Aside from the onerous preparation requirements, endoscopic evaluation also carries increased patient risks, including anesthetic and procedural risks such as bleeding and perforation [7]. Further technical limitations of endoscopy include limited access to the small bowel with often only the distal 10–15 cm of the terminal ileum visualized with standard colonoscopes.
These challenges emphasize the need for alternate, less invasive surrogate markers of disease activity such as magnetic resonance enterography (MRE) as recommended by European Crohn and Colitis Organisation guidelines as the test of choice for the diagnosis and staging of patients with small bowel CD [6]. Studies have demonstrated that MRE is both accurate and highly correlates with endoscopic evaluation in the assessment of small bowel CD with a recent meta-analysis demonstrating pooled sensitivity and specificity for MRE in detecting active small bowel CD of 87.9% (95% confidence interval, 81.8%–92.5%) and 81.2% (95% confidence interval, 71.9%–88.4%) respectively [8-11]. In an attempt to standardize reporting, multiple MRE indices of CD activity have been developed, including most recently with the simplified magnetic resonance index of activity (sMaRIA) [8]. While these tools are a welcome attempt to standardize reporting of disease activity, there are inherent limitations with published indices, including the non-standardization of MRE protocols relating to variable administration of contrast and bowel distention media, rectal instillation of water, bowel cleansing, as well as potential exclusion of poorer quality MREs in the original studies which limit their utility in clinical practice [8,9]. The Society of Abdominal Radiology CD Disease-Focused Panel (SAR-CD-DFP), the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), and the European Society of Paediatric Radiology (ESPR) have produced recommendations to optimize MRE image acquisition for CD assessment [12,13]. Generally, these consist of ingestion of 1,000–1,500 mL of biphasic oral contrast, administration of timed antiperistalsis agents and intraprocedural breath holding [14,15] to achieve adequate bowel distention and reduce motion artifact. Previous studies have demonstrated that definitions of optimal bowel distention and motion artifact are poorly described in the literature with no clear expert consensus [16]. Optimization of these 2 key parameters of quality would likely improve the accuracy of MRE in small bowel CD but have never been directly studied.
The primary aims of this study were: (1) to assess the quality of MRE studies as a composite of both motion artifact and bowel distention, and (2) subsequently assess the impact of quality of MRE in discriminating between active and inactive disease utilizing MRE activity indices in patients with small bowel CD. Secondary aims were (1) to calculate the proportion of poor-quality MREs performed across 2 tertiary Australian IBD centers, and (2) to quantify the degree to which bowel distention and motion artifact individually affect the discrimination between active and inactive disease on MRE activity indices in patients with small bowel CD.
METHODS
1. Study Design
A multicenter retrospective cohort study was conducted across 2 tertiary IBD centers in Australia. Inclusion criteria included the following: (1) adult patients 16 years or older with, (2) histologically proven, ileal or ileocolonic (Montreal L1 or L3 location) CD who underwent, (3) tandem CD activity assessment with MRE and colonoscopy within 30 days of each other. Patients who had previously had a surgical resection of the small and/or large bowel were included as long as they met the other inclusion criteria. Exclusion criteria included the following: (1) patients who underwent colonoscopy without successful intubation of the terminal ileum, (2) MRE in which a completion of all image sequences was not possible, and (3) MRE in which patients were unable to consume the required volume and/or have the required antispasmodic agents. Data comprising MRE, endoscopic, relevant clinical, and surgical information were collected over 6 years between October 2014 to January 2021 inclusive. MREs conducted in this period were identified through radiology databases at both centers and cross-checked with endoscopy databases, capturing those who had a colonoscopy with ileal intubation within 30 days of the MRE. This project was approved as a quality assurance activity by the institutional office of ethics (reference number: QA19/024). Informed consent was waived.
2. Colonoscopy Protocol
Colonoscopy was performed using standard bowel preparation as per local protocols under anesthetist-administered deep sedation, with Olympus 190 series high-definition colonoscopes by Gastroenterologists accredited by the Conjoint Committee for the Recognition of Training in Gastrointestinal Endoscopy (CCRTGE) of Australia. Colonoscopy reporting was performed using Olympus Endobase© software (Olympus, Tokyo, Japan). CD activity was reported segmentally in real-time upon visual inspection using the Simplified Endoscopic Score for CD (SES-CD).
3. MRE Protocol
MRE scans were performed across 2 tertiary IBD centers using a 1.5T (Siemens Magnetom Aera, Erlangen, Germany) and a 3T (Philips Ingenia, Best, The Netherlands) machine respectively. The respective MRE protocols followed principles from previously published expert consensus statements [12,13]. All patients were fasted for a minimum of 8 hours prior to arrival for MRE in line with institutional protocols. Following arrival, patients ingested 1,000–2,000 mL sorbitol or psyllium-based biphasic oral contrast in the preceding 45 to 120 minutes which has previously been shown to produce comparable bowel distension in MRE [17]. In patients with previous significant small bowel resection or end ileostomy, the volume of contrast was ingested within 30 minutes as determined by the supervising abdominal radiologist. Specifically in patients with an end ileostomy, the stoma was plugged prior to contrast ingestion. Patients received intravenous antiperistalsis agents (hyoscine butylbromide or glucagon if contraindication to hyoscine butylbromide) prior to image acquisition. Detailed MRE preparation and imaging sequence acquisition protocols for both magnetic resonance machines used to acquire images are provided in Supplementary Table 1. All MRE were performed in a prone position unless not feasible.
4. Further Endoscopic Data Considerations
Given this study was focused on small bowel CD, only the ileal SES-CD was required for the purposes of data extraction with scores ≥ 3 used to discriminate between active and inactive disease. In addition, mild disease was defined as an SES-CD between 3–6 points and moderate disease between 7–15 points. Each colonoscopy was independently reviewed with ileal segments rescored by one of the investigators who is also CCRTGE accredited in colonoscopy, to validate the accuracy of the original ileal SES-CD score. This reassessment was performed based upon descriptors in the report as well as review of the ileal image(s). Where there was discordance between the initial endoscopist’s score and the reviewer, a second CCRTGE accredited reviewer independently assessed the colonoscopy to reach a consensus with the original endoscopist’s independent SES-CD scoring.
5. Further MRE Data Considerations
Ileal segments of small bowel were independently scored for CD activity by a Royal Australian and New Zealand College of Radiologists (RANZCR) certified radiologist/s blinded to endoscopic data who has 11 years of abdominal radiology experience. Ileal CD activity was scored using 4 validated MRE disease activity indices; MaRIA, sMaRIA, CD MRE index (CDMI), and the London index [8,9,18]. Based on previously validated cutoffs, “active ileal CD” was defined as; MaRIA score ≥ 7 ( ≥ 11 being severe disease), sMaRIA score ≥ 1, CDMI ≥ 3, and London index ≥ 4.1 [18,19].
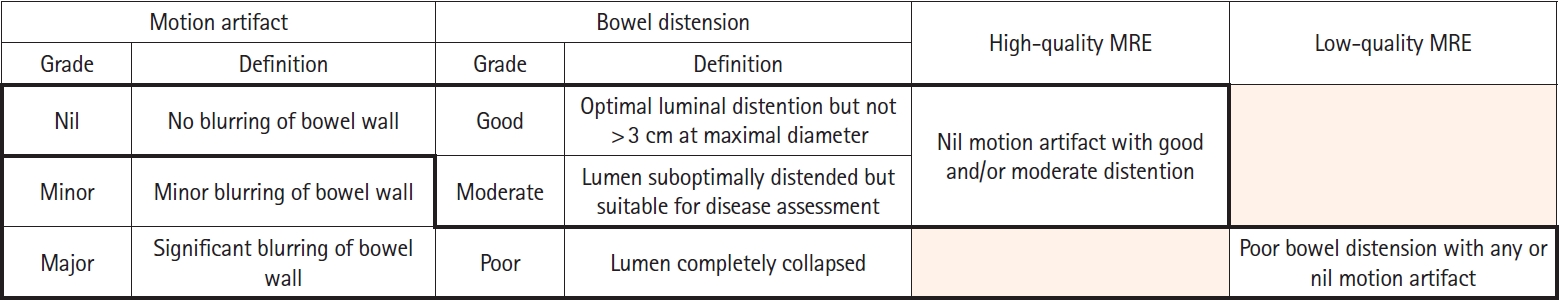
Due to lack of consensus definitions, there is significant heterogeneity in MRE image quality descriptors [16]. In our study, MRE image quality was defined across 2 parameters: (1) motion artifact and (2) bowel distention. Grading was performed in proximal, mid, and distal small bowel segments. Each parameter was graded using a 3-point scale. A summary of the grading across both parameters is summarized in Fig. 1. Bowel distension was visually graded per the following definitions: poor: lumen completely collapsed, moderate: lumen distension suboptimal but suitable for disease assessment, good: optimal luminal distention but not > 3 cm at maximal diameter. Motion artifact was visually graded as per the following definitions: nil: no blurring of bowel wall, minor: minor blurring of bowel wall, marked: significant blurring of bowel wall. Examples of grading are illustrated in Figs. 2-5. Thirty-eight out of 137 scans (28%) were randomly allocated to a second RANZCR-certified radiologist with 15 years of abdominal radiology experience for grading of motion artifact and bowel distension in the distal small bowel with interpretation performed blinded to the original radiologist (N.K.).
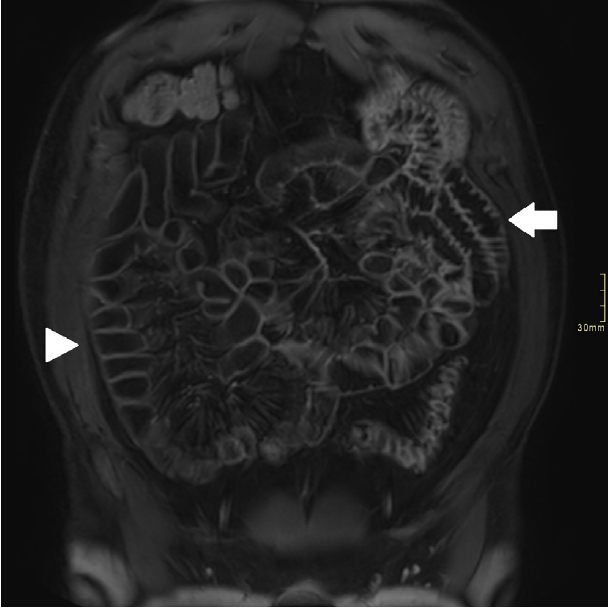
Coronal T1 post-contrast sequence showing poor distension and marked movement artifact in proximal small bowel (arrow) and good distension and minor movement artifact in distal small bowel (arrowhead).

(A) Coronal T2 sequence showing a long segment of inflammatory disease in distal small bowel (arrowhead) with high T2 signal in bowel wall and adjacent fat. (B) Corresponding coronal T1 post-contrast sequence showing poor distension and mark (arrow).
The quality of images was dependent on the grade of quality seen across bowel distention and motion artifact in the distal small bowel. High-quality images were defined as nil motion artifact and good and/or moderate bowel distention. All other combinations of motion artifact and bowel distension images were defined as poor quality. Furthermore, all images with poor bowel distension in the distal small bowel were defined as a poor quality (Fig. 1).
6. Statistical Analyses
Normally distributed variables were expressed as means with standard deviations, while skewed variables were expressed as medians with interquartile range. Categorical variables were expressed as frequencies and percentages. The discriminative performance of various scores were evaluated using receiver operator characteristic (ROC) curves and the area under the curve (AUC). Statistical comparison of the AUCs of different scores was performed using the DeLong method [20]. Figures of smooth ROC curves were generated using parametric ROC estimation using a probit model [21]. A two-sided P-value of < 0.05 was considered statistically significant. Interobserver variability was tested using the kappa statistic. Stata/IC 16 (College Station, TX, USA, 2020) was used for analysis.
RESULTS
1. Baseline Population Data
In 820 patients were identified through initial screening with 137 patients meeting inclusion criteria with tandem MRE and colonoscopy performed within 30 days of each other. The median time between MRE and colonoscopy was 16 days (range, 0–30 days). Of these, 34 patients (24.8%) had prior bowel resections at the time of inclusion into this study, with ileocaecal resection previously performed in 15 out of 34 patients (44.1%) and isolated ileal resection in 8 out of 34 patients (23.5%). Endoscopically active disease, defined by a SES-CD of ≥ 3 was seen in 64 (46.7%) patients with 48 (35.0%) exhibiting mild activity and 16 (11.8%) moderate activity as per SES-CD scores within the ileum. MRE disease activity represented through the sMaRIA showed active disease (sMaRIA ≥ 1) in 63 patients (46.0%). Other indices of disease activity are represented in Table 1.
2. MRE Quality Parameters
There were 137 ileal/distal small bowel segments assessed on MRE, 93 (67.9%) to be of high quality as defined by nil motion artifact plus good and/or moderate bowel distention. Additionally, 44 (32.1%) were considered low quality due to either the presence of any motion artifact or any motion grading plus poor bowel distention. Of the 44 low-quality MRE scans, 32 (72.7%) comprised any motion artifact with moderate/good bowel distension, 6 (13.6%) comprised either poor-quality bowel distention plus minor or major motion artifact and the remaining 6 (13.6%) all exhibited poor-quality bowel distention with no motion artifact. There was a substantial agreement in 34 out of 38 (89%) distal small bowel segments for motion artifact grading between both radiologists (κ= 0.73). There was a substantial agreement in 33 out of 38 (87%) of distal small bowel segments for bowel distension grading between both radiologists (κ= 0.78). Using the same MRE grading methods, the proximal and mid small bowel segments of the 137 MRE studies were also assessed for image quality. Only 60 (43.8%) and 18 (13.1%) of mid and proximal small bowel segments respectively were of high quality compared to 93 (67.8%) of distal ileal segments on MRE. A summary of the quality parameters is provided in Table 2.
3. Discrimination between Active/Inactive Diseases upon Quality of MRE
Using validated cutoffs for CD endoscopic and MRE disease activity indices, the MaRIA, sMaRIA, and CDMI demonstrated a good ability to discriminate between inactive and inactive distal small bowel disease when compared to endoscopic examination on ROC analysis and the London index achieved a fair performance (MaRIA AUC 0.838, sMaRIA AUC 0.834, CDMI AUC 0.850, and London AUC 0.748). Within the low-quality MRE cohort, the performance of MRE activity indices in discriminating between active and inactive endoscopic disease dropped significantly (P< 0.05) across all assessed MRE indices of activity on ROC analysis (Table 3). The MaRIA score had poor discriminative power (MaRIA AUC 0.634) and the remaining MRE indices failed in their ability to discriminate between active and inactive disease (sMaRIA AUC 0.527, CDMI AUC 0.595, and London AUC 0.511) (Table 3).
4. Subanalysis of Individual Quality Parameters
There were 38 (27.7%) distal small bowel MRE segments affected by motion artifact (Table 2). In distal small bowel segments not affected by motion artifact, the MaRIA, sMaRIA, and CDMI demonstrated a good ability to discriminate between inactive and inactive disease on ROC analysis (MaRIA AUC 0.829, sMaRIA AUC 0.814, and CDMI AUC 0.838) with the London index achieving a fair performance (AUC 0.723) (Table 4). Within the distal small bowel segments affected by motion artifact, the performance of MRE activity indices in discriminating between active and inactive endoscopic disease dropped significantly (P< 0.05), with the sMaRIA and CDMI scores failing to discriminate between active and inactive disease (sMaRIA AUC 0.544, CDMI AUC 0.598). The MaRIA had a reduced ability to discriminate between endoscopically active and inactive disease but did not reach statistical significance (MaRIA AUC 0.631, P= 0.06) (Table 4). In distal small bowel segments with good bowel distension, all MRE indices of activity maintained a good or fair ability to discriminate between inactive and inactive disease on ROC analysis (MaRIA AUC 0.803, sMaRIA AUC 0.759, CDMI AUC 0.789, and London AUC 0.723). Whilst the AUC was generally lower with moderate or poor bowel dilatation compared with good bowel distention, there were no statistically significant differences elicited by any of the MRE indices (Supplementary Table 2).
DISCUSSION
This is the first study to directly assess the impact of image quality metrics on CD activity assessment by comparing established MRE CD activity indices against the gold standard of ileocolonoscopy. Furthermore, our study has demonstrated the substantial proportion of suboptimal MREs performed in a tertiary real-world setting, signifying the magnitude of this unheralded clinical issue.
In this cohort, approximately one-third of ileal segments in MRE’s were deemed as low quality. Our subanalysis demonstrated a significant reduction in discriminative ability between active and inactive disease by MRE in the presence of any motion artifact. There was also apparent numerical trends of reduced discrimination capacity with poor bowel distention. The high prevalence of low-quality scans in our study is of concern as the study centers follow the principles of MRE protocols recommended by SAR-CD-DFP and ESGAR/ESPR [12,13], hence are likely representative of the variable quality of scans performed globally. The further drop-off in quality seen in the more proximal small bowel segments, however, is not surprising given that MRE protocols are tailored to assessing the distal small bowel.
Hence, given that in setting of low-quality images, MRE did not discriminate well between active and inactive disease (the original MaRIA performed poorly and all other indices failed in discrimination capacity, each P< 0.05), these scans should be interpreted with caution. This has direct implications on the applicability of such indices of CD activity which assume interpretable MRE scans and in turn, casts doubt on the accuracy of clinical decision making in this context. Within the development studies for the MaRIA and sMaRIA, multiple additional steps were taken to optimize image quality such as bowel cleansing and rectal instillation of water [8,9] but these are not typically performed in real-world clinical scenarios given they are time-consuming, add cost and are poorly tolerated by patients [22].
On subanalysis of individual metrics, the presence of any motion artifact showed a significant reduction in the sMaRIA which failed to discriminate active and inactive disease and there was a trend towards poor discriminative capacity with the MaRIA (P= 0.06). There was also a numerically lower (albeit insignificant) discrimination capacity with moderate/poor compared with good bowel distension. These findings imply that motion artifact exerts a greater impact on image quality and CD activity assessment than suboptimal bowel distention. Further investigation into effective means of negating motion artifact is therefore required. Antiperistalsis agents are used to reduce motion artifact by preventing movement of normally peristalsis small bowel loops though the optimal dosing and delivery method (i.e., intravenous vs. subcutaneous) has yet to be determined [23,24]. Breath holding is also performed prior to specific MRE image sequences with studies showing diminished respiratory motion artifact in abdominal magnetic resonance imaging with end expiratory breath holding [25].
This study has some limitations and weaknesses. First, the data were retrospectively acquired, therefore open to inherent biases in this context, including that the directionality of associations between variables cannot be ascertained. Second, there was a median period of 16 days between MRE and ileocolonoscopy which could result in discrepancies in activity assessment between the modalities. Indeed, there is also inherent shortcomings of attributing ileocolonoscopy as the gold standard, given that unlike MRE, it cannot assess more proximal or transmural disease. Third, due to the lack of published data and/or expert guidelines in this space, the definitions and grading of bowel distension and motion artifact were somewhat arbitrary and/or based upon local radiologist experience. Other studies previously examining quality metrics in MRE have addressed this by applying a similar, pragmatic approach [26-28]. Fourth, whilst diffusion-weighted imaging (DWI) is now routinely performed at our centers as part of MRE this study did not evaluate MRE indices that include DWI parameters such as the Clermont [10] as DWI was not performed in some of the older MRE sequences. Therefore, the impact of image quality on DWI parameters accuracy was unable to be determined through this study. Fifth, due to image optimization for small bowel only, assessment of image quality on disease activity within colonic segments was not possible with further studies required with MRE.
In conclusion, despite marked technological advances in recent decades, the assessment of small bowel CD activity remains challenging and both MRE and ileocolonoscopy have inherent shortcomings. The importance of quality assurance and the impact of poor quality on clinical outcomes is well established with respect to colonoscopy, yet the impact of quality of MRE has received minimal attention. This study has clearly shown that many MREs performed in typical high-volume IBD centers may be of suboptimal quality and that poor-quality MREs have a significantly reduced capacity to discriminate between active and inactive ileal CD. This has major implications for clinical decision making with MRE of low quality ultimately requiring either repeating the MRE with individualized optimization of technique including enteroclysis or recommend recommendation for alternate imaging modality assessment.
Moving forward, the scale of poor-quality MRE’s needs to be further elucidated and replicated in other real-world settings. Moreover, prospective studies should seek to validate this study’s findings, with the ultimate goal of establishing a quality grading system, incorporating motion artifact and bowel wall distention for MRE, thus enhancing the utility and outcomes arising from this integral imaging technique.
Notes
Funding Source
Bohra A received an Australian Government Research Training Program Scholarship.
Conflict of Interest
Segal JP has received speaker fees from Janssen, Takeda and AbbVie and an unrestricted research grant from Tillotts. Van Langenberg DR has received speaker fees from Janssen, Takeda, Pfizer, is on the advisory board for Janssen, Takeda, Pfizer, AbbVie and has research support from Janssen, Medtronic and Pfizer. No other potential conflicts of interest relevant to this article were reported.
Data Availability Statement
The data underlying this article will be shared on a reasonable request to the corresponding author.
Author Contributions
Conceptualization: Bohra A, Connoley DJ. Data curation: Bohra A, Connoley DJ. Formal analysis: Bohra A, Con D, Segal JP, Kutaiba N. Investigation; Methodology; Project administration; Software: Bohra A. Supervision: Niewiadomski O, Vasudevan A, Van Langenberg DR, Kutaiba N. Validation: Bohra A. Writing - original draft: Bohra A. Writing - review & editing: Bohra A, Vasudevan A, Van Langenberg DR, Kutaiba N. Approval of final manuscript: all authors.
Supplementary Material
Supplementary materials are available at the Intestinal Research website (https://www.irjournal.org).
Supplementary Table 1.
Magnetic Resonance Enterography Protocols
Supplementary Table 2.
Performance of MRE Scores in Discriminating Active Disease (SES-CD ≥3) as Measured by AUC, Stratified by Degree of Bowel Distention