|
 |
- Search
| Intest Res > Volume 22(2); 2024 > Article |
|
Abstract
Background/Aims
Methods
Results
ADDITIONAL INFORMATION
Conflict of Interest
Segal JP has received speaker fees from Janssen, Takeda and AbbVie and an unrestricted research grant from Tillotts. Van Langenberg DR has received speaker fees from Janssen, Takeda, Pfizer, is on the advisory board for Janssen, Takeda, Pfizer, AbbVie and has research support from Janssen, Medtronic and Pfizer. No other potential conflicts of interest relevant to this article were reported.
Data Availability Statement
The data underlying this article will be shared on a reasonable request to the corresponding author.
Author Contributions
Conceptualization: Bohra A, Connoley DJ. Data curation: Bohra A, Connoley DJ. Formal analysis: Bohra A, Con D, Segal JP, Kutaiba N. Investigation; Methodology; Project administration; Software: Bohra A. Supervision: Niewiadomski O, Vasudevan A, Van Langenberg DR, Kutaiba N. Validation: Bohra A. Writing - original draft: Bohra A. Writing - review & editing: Bohra A, Vasudevan A, Van Langenberg DR, Kutaiba N. Approval of final manuscript: all authors.
Supplementary Material
Supplementary Table 1.
Supplementary Table 2.
Fig. 2.
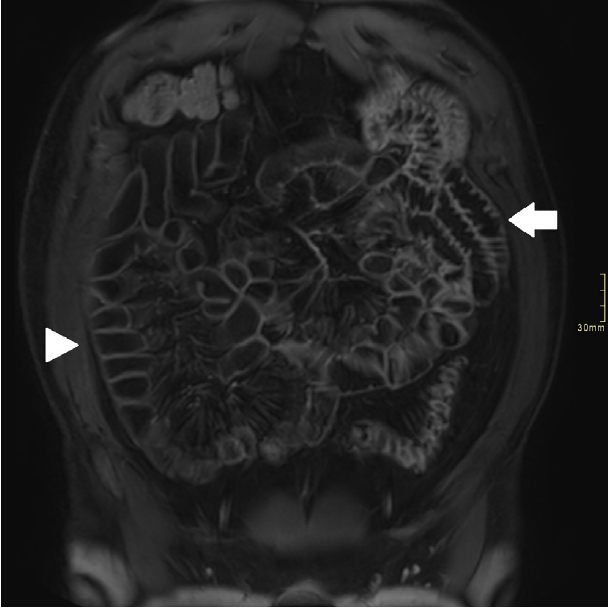
Fig. 3.

Fig. 4.

Fig. 5.

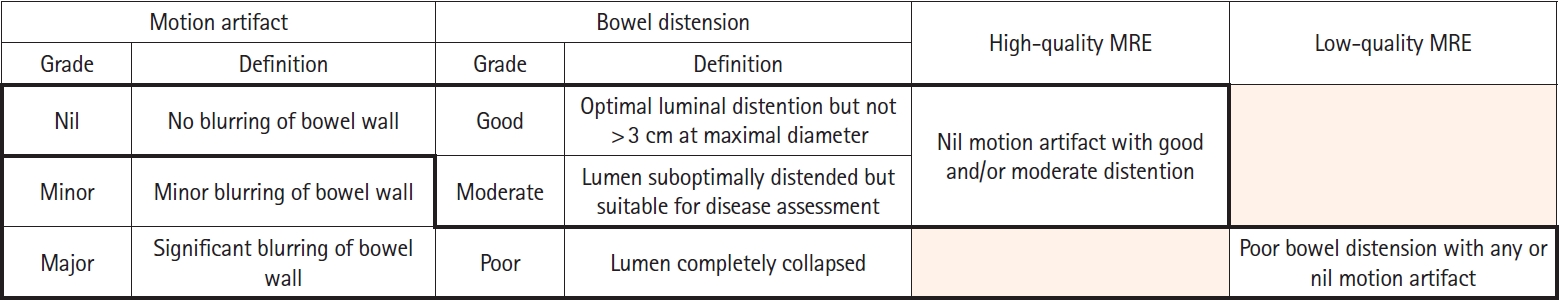
Table 1.
Table 2.
| Parameter | No. (%) |
|---|---|
| High qualitya | |
| Distal/ileal segment | 93 (67.8) |
| Mid small bowel segment | 60 (43.8) |
| Proximal small bowel segment | 18 (13.1) |
| Low qualityb | |
| Distal/ileal segment | 44 (32.1) |
| Mid small bowel segment | 77 (56.2) |
| Proximal small bowel segment | 119 (86.9) |
| Motion artifact | |
| Proximal small bowel | |
| Nil | 30 (21.9) |
| Minor | 69 (50.4) |
| Major | 38 (27.7) |
| Mid small bowel | |
| Nil | 65 (47.4) |
| Minor | 59 (43.1) |
| Major | 13 (9.5) |
| Distal small bowel | |
| Nil | 99 (72.3) |
| Minor | 31 (22.6) |
| Major | 7 (5.1) |
| Bowel distention | |
| Proximal small bowel | |
| Good | 14 (10.2) |
| Moderate | 45 (32.8) |
| Poor | 78 (56.9) |
| Mid small bowel | |
| Good | 62 (45.3) |
| Moderate | 50 (36.5) |
| Poor | 25 (18.2) |
| Distal small bowel | |
| Good | 81 (59.1) |
| Moderate | 44 (32.1) |
| Poor | 12 (8.8) |