|
 |
- Search
| Intest Res > Volume 21(4); 2023 > Article |
|
Abstract
Background/Aims
Methods
Results
ADDITIONAL INFORMATION
Funding Source
The work was supported by a grant (21153MFDS601) from Ministry of Food and Drug Safety in 2022.
Author Contributions
Conceptualization: Cha JM. Data curation: Kang HS, Jeon SH, Park SB. Formal analysis: Kang HS, Yoon JY, Kwak MS. Funding acquisition: Cha JM. Methodology: Yoon JY, Kwak MS, Cha JM. Supervision: Cha JM. Writing - original draft: Kang HS, Cha JM. Writing - review & editing: Cha JM. Approval of final manuscript: all authors.
Supplementary Material
Supplementary Table 1.
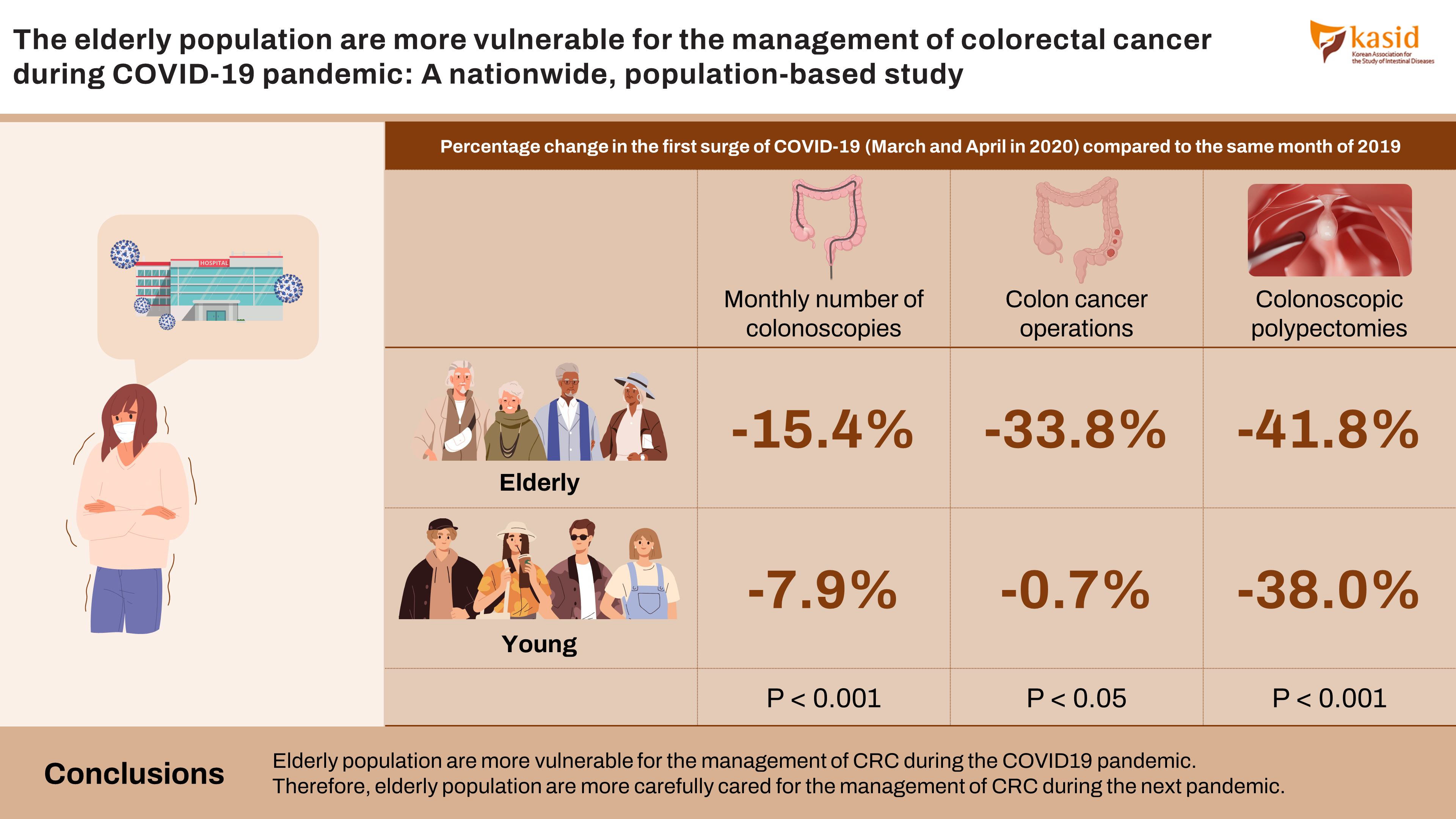
Fig. 1.
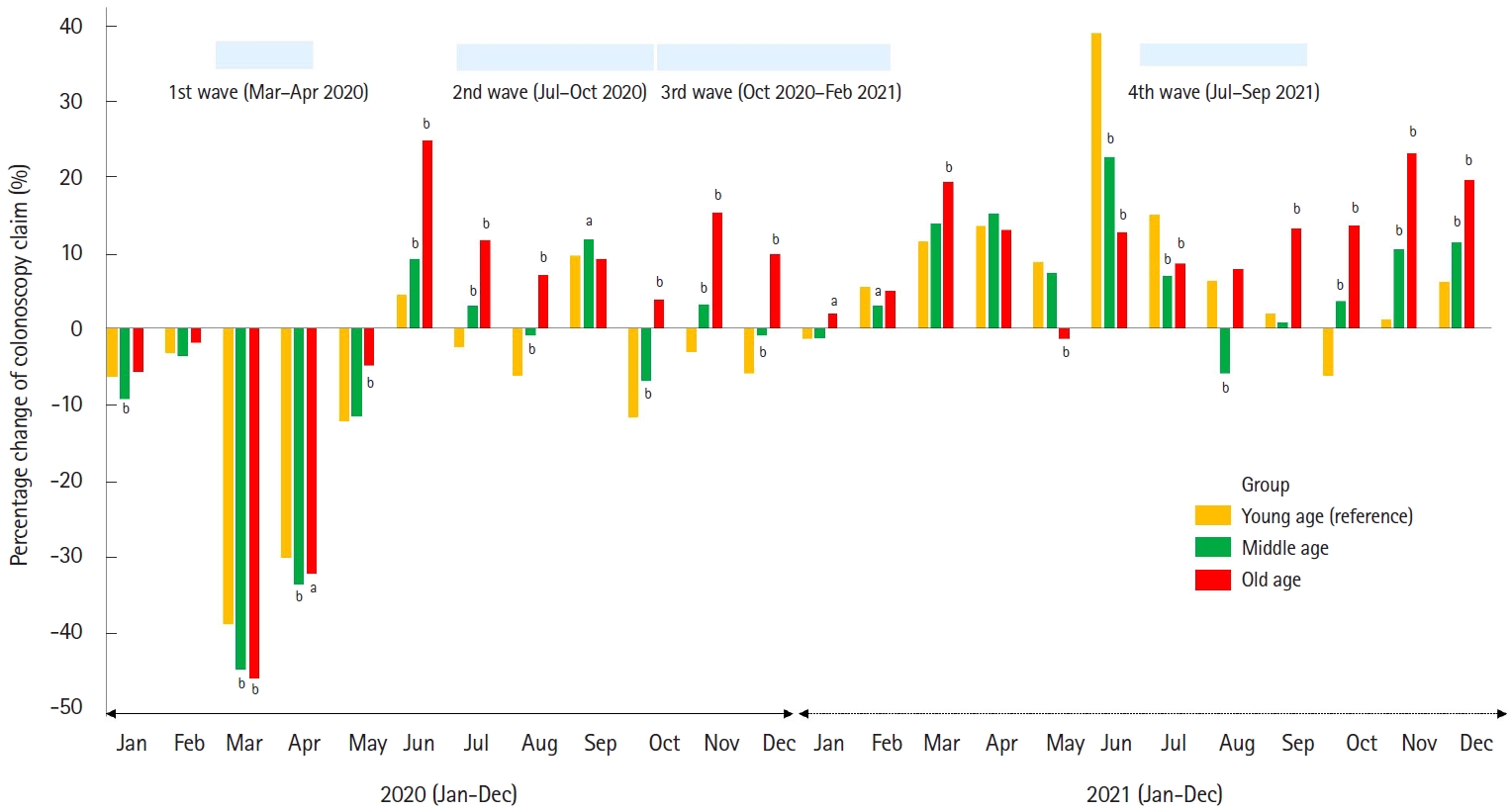
Fig. 2.

Fig. 3.
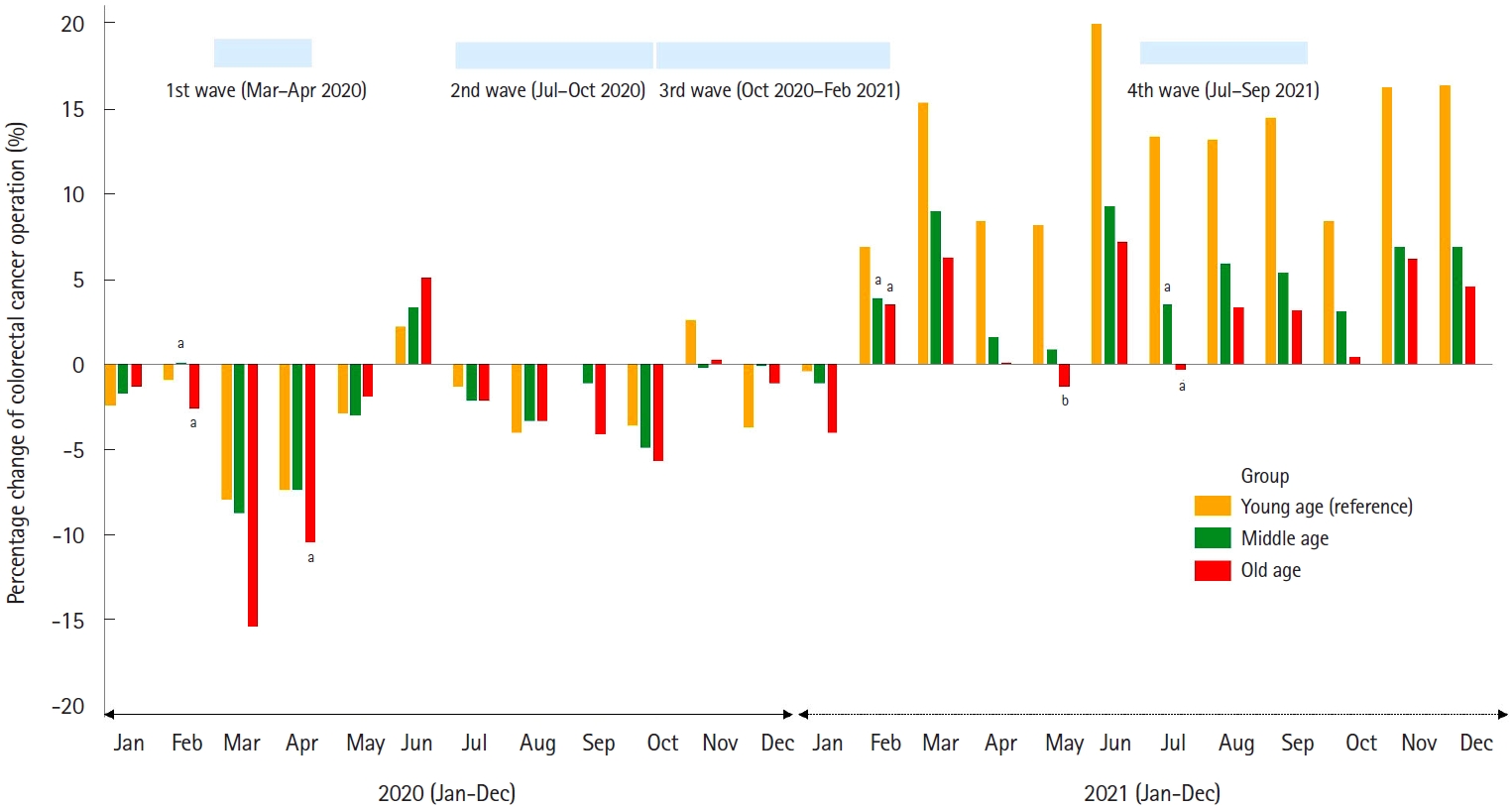
Fig. 4.
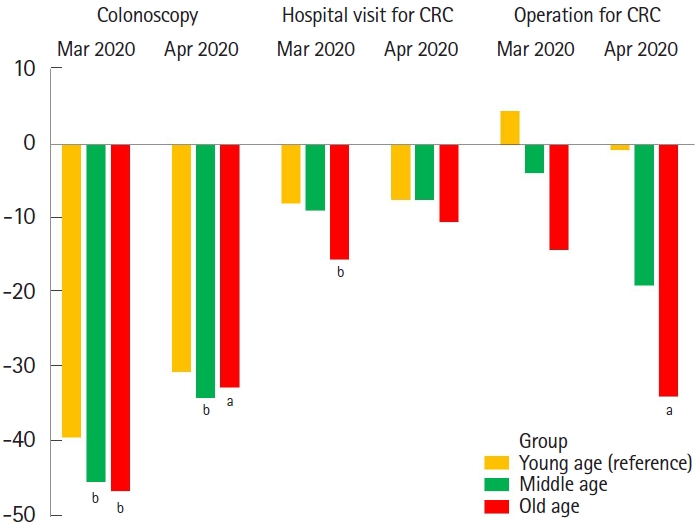
Table 1.
| Group | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | Total | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Young age | |||||||||||||||
| 2019 | 46,502 | 37,854 | 41,126 | 41,725 | 40,790 | 39,623 | 46,073 | 48,838 | 41,409 | 51,223 | 61,418 | 66,936 | 563,517 | ||
| 2020 | 43,474 | 36,606 | 24,972 | 28,983 | 35,736 | 41,383 | 44,894 | 45,751 | 45,371 | 45,104 | 59,437 | 62,914 | 514,625 | ||
| Change (%)b | -6.5 | -3.3 | -39.3 | -30.5 | -12.4 | +4.4 | -2.6 | -6.3 | +9.6 | -11.9 | -3.2 | -6.0 | -8.7 | ||
| 2021 | 45,815 | 39,894 | 45,818 | 47,349 | 44,327 | 55,123 | 53,006 | 51,858 | 42,190 | 47,982 | 62,119 | 70,987 | 606,468 | ||
| Change (%)b | -1.5 | +5.4 | +11.4 | +13.5 | +8.7 | +39.1 | +15.0 | +6.2 | +1.9 | -6.3 | +1.1 | +6.1 | +7.6 | ||
| Middle age | |||||||||||||||
| 2019 | 76,230 | 63,451 | 80,500 | 80,814 | 79,534 | 74,638 | 87,650 | 89,389 | 71,612 | 94,330 | 103,402 | 105,251 | 1,006,801 | ||
| 2020 | 68,986 | 61,109 | 44,025 | 53,374 | 70,139 | 81,469 | 90,216 | 88,460 | 80,006 | 87,673 | 106,584 | 104,237 | 936,278 | ||
| Change (%)b | -9.5d | -3.7e | -45.3d | -34.0d | -11.8e | +9.2d | +2.9d | -1.0d | +11.7c | -7.1d | +3.1d | -1.0d | -7.0d | ||
| 2021 | 75,182 | 65,260 | 91,606 | 93,098 | 85,321 | 91,612 | 93,734 | 84,013 | 72,135 | 97,644 | 114,145 | 117,154 | 1,080,904 | ||
| Change (%)b | -1.4e | +2.9c | +13.8e | +15.2e | +7.3e | +22.7d | +6.9d | -6.0d | +0.7e | +3.5d | +10.4d | +11.3d | +7.4e | ||
| Old age | |||||||||||||||
| 2019 | 18,712 | 15,713 | 23,306 | 24,160 | 22,904 | 20,338 | 22,196 | 18,593 | 17,319 | 22,693 | 21,205 | 20,082 | 247,221 | ||
| 2020 | 17,626 | 15,398 | 12,480 | 16,277 | 21,761 | 25,378 | 24,776 | 19,896 | 18,895 | 21,852 | 24,442 | 22,054 | 240,835 | ||
| Change (%)b | -5.8e | -2,.0e | -46.5d | -32.6c | -5.0d | +24.8d | +11.6d | +7.0d | +9.1e | +3.7d | +15.3d | +9.8d | -2.6d | ||
| 2021 | 19,065 | 16,486 | 27,805 | 27,301 | 22,566 | 22,914 | 24,086 | 20,047 | 19,610 | 25,788 | 26,121 | 24,024 | 275,813 | ||
| Change (%)b | +1.9c | +4.9e | +19.3d | +13.0e | -1.5d | +12.7d | +8.5d | +7.8e | +13.2d | +13.6d | +23.2d | +19.6d | +11.6d | ||
Table 2.
| Group | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | Total | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Young age | |||||||||||||||
| 2019 | 4,779 | 4,249 | 4,310 | 4,482 | 4,316 | 4,294 | 4,535 | 4,448 | 4,303 | 4,576 | 4,491 | 4,590 | 53,373 | ||
| 2020 | 4,663 | 4,212 | 3,969 | 4,149 | 4,191 | 4,388 | 4,476 | 4,271 | 4,301 | 4,410 | 4,609 | 4,759 | 52,398 | ||
| Change (%)b | -2.4 | -0.9 | -7.9 | -7.4 | -2.9 | +2.2 | -1.3 | -4.0 | 0.0 | -3.6 | +2.6 | -3.7 | -1.8 | ||
| 2021 | 4,759 | 4,541 | 4,973 | 4,860 | 4,671 | 5,155 | 5,141 | 5,034 | 4,927 | 4,957 | 5,221 | 5,341 | 59,580 | ||
| Change (%)b | -0.4 | +6.9 | +15.4 | +8.4 | +8.2 | +20.1 | +13.4 | +13.2 | +14.5 | +8.3 | +16.3 | +16.4 | +11.6 | ||
| Middle age | |||||||||||||||
| 2019 | 25,931 | 23,214 | 24,638 | 24,965 | 24,592 | 24,011 | 25,455 | 24,158 | 23,841 | 25,323 | 24,951 | 25,553 | 296,632 | ||
| 2020 | 25,487 | 23,242 | 22,487 | 23,122 | 23,842 | 24,835 | 24,908 | 23,354 | 23,575 | 24,071 | 24,893 | 25,534 | 289,350 | ||
| Change (%)b | -1.7e | +0.1e | -8.7e | -7.4e | -3.0e | +3.4e | -2.1e | -3.3e | -1.1e | -4.9e | -0.2e | -0.1e | -2.5e | ||
| 2021 | 25,634 | 24,117 | 26,846 | 25,367 | 24,813 | 26,250 | 26,338 | 25,573 | 25,118 | 26,103 | 26,673 | 27,322 | 310,154 | ||
| Change (%)b | -1.1e | +3.9e | +9.0c | +1.6c | +0.9c | +9.3d | +3.5d | +5.9c | +5.4d | +3.1c | +6.9d | +6.9d | +4.6d | ||
| Old age | |||||||||||||||
| 2019 | 19,475 | 17,473 | 19,205 | 19,825 | 19,272 | 18,810 | 19,987 | 18,745 | 18,653 | 20,035 | 18,984 | 19,199 | 229,663 | ||
| 2020 | 19,220 | 17,027 | 16,244 | 17,757 | 18,906 | 19,760 | 19,577 | 18,120 | 17,890 | 18,891 | 19,044 | 18,986 | 221,422 | ||
| Change (%)b | -1.3e | -2.6e | -15.4d | -10.4e | -1.9e | +5.1e | -2.1e | -3.3e | -4.1e | -5.7e | +0.3e | -1.1c | -3.6c | ||
| 2021 | 18,700 | 18,093 | 20,415 | 19,841 | 19,021 | 20,156 | 19,936 | 19,391 | 19,256 | 20,117 | 20,162 | 20,080 | 235,168 | ||
| Change (%)b | -4.0e | +3.5e | +6.3d | +0.1d | -1.3d | +7.2d | -0.3d | +3.4d | +3.2d | +0.4d | +6.2d | +4.6d | +2.4d | ||
Table 3.
| Group | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | Total | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Young age | |||||||||||||||
| 2019 | 192 | 161 | 157 | 147 | 167 | 162 | 152 | 175 | 159 | 146 | 160 | 154 | 1,932 | ||
| 2020 | 168 | 145 | 164 | 146 | 177 | 167 | 166 | 154 | 162 | 164 | 149 | 154 | 1,916 | ||
| Change (%)b | -12.5 | -9.9 | +4.5 | -0.7 | +6.0 | +3.1 | +9.2 | -12.0 | +1.9 | +12.3 | -6.9 | 0.0 | -0.8 | ||
| 2021 | 197 | 118 | 197 | 156 | 160 | 157 | 180 | 168 | 153 | 160 | 164 | 148 | 1,958 | ||
| Change (%)b | 2.6 | -26.7 | +25.5 | +6.1 | -4.2 | -3.1 | +18.4 | -4.0 | -3.8 | +9.6 | +2.5 | -3.9 | +1.3 | ||
| Middle age | |||||||||||||||
| 2019 | 1,030 | 773 | 928 | 814 | 803 | 734 | 878 | 734 | 770 | 707 | 797 | 825 | 9,793 | ||
| 2020 | 956 | 949 | 893 | 660 | 708 | 760 | 759 | 690 | 700 | 745 | 821 | 809 | 9,450 | ||
| Change (%)b | -7.2e | +22.8c | -3.8e | -18.9e | -11.8e | +3.5e | -13.6e | -6.0e | -9.1e | +5.4e | +3.0e | -1.9e | -3.5e | ||
| 2021 | 972 | 828 | 938 | 807 | 777 | 822 | 787 | 828 | 689 | 843 | 873 | 827 | 9,991 | ||
| Change (%)b | -5.6e | +7.1c | +1.1e | -0.9e | -3.2e | +12.0e | -10.4c | +12.8e | -10.5e | +19.2e | +9.5e | +0.2e | +2.0e | ||
| Old age | |||||||||||||||
| 2019 | 789 | 608 | 766 | 773 | 757 | 666 | 765 | 661 | 585 | 621 | 641 | 628 | 8,260 | ||
| 2020 | 643 | 709 | 658 | 512 | 683 | 736 | 685 | 585 | 631 | 649 | 661 | 626 | 7,778 | ||
| Change (%)b | -18.5e | +16.6c | -14.1e | -33.8c | -9.8e | +10.5e | -10.5e | -11.5e | +7.9e | +4.5e | +3.1e | -0.3e | -5.8e | ||
| 2021 | 755 | 607 | 809 | 726 | 707 | 722 | 702 | 771 | 628 | 711 | 682 | 664 | 8,484 | ||
| Change (%)b | -4.3e | -0.2c | +5.6e | -6.1e | -6.6d | +8.4e | -8.2c | +16.6e | +7.4e | +14.5e | +6.4e | +5.7e | +2.7e | ||
a Operations for colorectal cancer was defined as colectomy (QA671, QA672, QA673, QA679, Q2671, Q2672, Q2673, Q2679, Q1261, Q1262) and/or surgical resection of rectum/sigmoid colon (QA921, QA922, QA923, QA924, Q2921, Q2922, Q2923, Q2924, Q2927, Q9292, QA928, Q2928) in patients with colorectal cancer.
Table 4.
| Group | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | Total | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Young age | |||||||||||||||
| 2019 | 19,667 | 16,193 | 19,183 | 20,776 | 21,170 | 21,095 | 23,714 | 24,635 | 21,204 | 27,841 | 34,673 | 38,087 | 288,238 | ||
| 2020 | 20,669 | 18,578 | 13,000 | 15,836 | 19,726 | 24,052 | 26,861 | 27,022 | 28,507 | 29,829 | 40,072 | 43,074 | 307,226 | ||
| Change (%)b | +5.1 | +14.7 | -32.2 | -23.8 | -6.8 | 14.0 | 13.3 | 9.7 | 34.4 | 7.1 | 15.6 | 13.1 | +6.6 | ||
| 2021 | 27,176 | 23,032 | 28,545 | 31,424 | 30,679 | 38,345 | 36,220 | 36,182 | 30,651 | 36,415 | 47,912 | 54,991 | 421,572 | ||
| Change (%)b | +38.2 | +42.2 | +48.8 | +51.3 | +44.9 | +81.8 | +52.7 | +46.9 | +44.6 | +30.8 | +38.2 | +44.4 | +46.3 | ||
| Middle age | |||||||||||||||
| 2019 | 58,085 | 42,727 | 54,794 | 55,730 | 54,953 | 51,426 | 61,076 | 62,322 | 50,040 | 66,360 | 75,486 | 79,342 | 712,341 | ||
| 2020 | 58,234 | 45,538 | 33,979 | 41,481 | 54,486 | 63,656 | 71,353 | 70,216 | 63,989 | 70,351 | 86,738 | 89,946 | 749,967 | ||
| Change (%)b | +0.3d | +6.6d | -38.0d | -25.6e | -0.8d | +23.8d | +16.8c | +12.7c | +27.9d | +6.0e | +14.9e | +13.4e | +5.3d | ||
| 2021 | 71,854 | 53,705 | 77,830 | 80,429 | 75,125 | 80,172 | 83,025 | 73,438 | 66,140 | 88,403 | 103,484 | 110,378 | 963,983 | ||
| Change (%)b | +23.7d | +25.7d | +42.0d | +44.3d | +36.7d | +55.9d | +35.9d | +17.8d | +32.2d | +33.2e | +37.1e | +39.1d | +35.3d | ||
| Old age | |||||||||||||||
| 2019 | 14,307 | 10,901 | 16,887 | 17,485 | 16,366 | 14,729 | 16,227 | 13,111 | 12,111 | 16,619 | 16,260 | 15,567 | 180,570 | ||
| 2020 | 14,649 | 11,804 | 9,836 | 12,992 | 17,295 | 19,807 | 19,740 | 15,618 | 15,525 | 17,476 | 20,182 | 19,053 | 193,977 | ||
| Change (%)b | +2.4e | +8.3d | -41.8d | -25.7e | +5.7d | +34.5d | +21.6d | +19.1d | +28.2c | +5.2e | +24.1d | +22.4d | +7.4e | ||
| 2021 | 17,856 | 13,490 | 23,705 | 23,719 | 19,366 | 19,426 | 20,761 | 16,569 | 16,663 | 22,881 | 23,643 | 22,208 | 240,287 | ||
| Change (%)b | +24.8d | +23.8d | +40.4d | +35.7d | +18.3d | +31.9d | +27.9d | +6.4d | +37.6d | +37.7d | +45.4d | +42.7e | +33.1d | ||