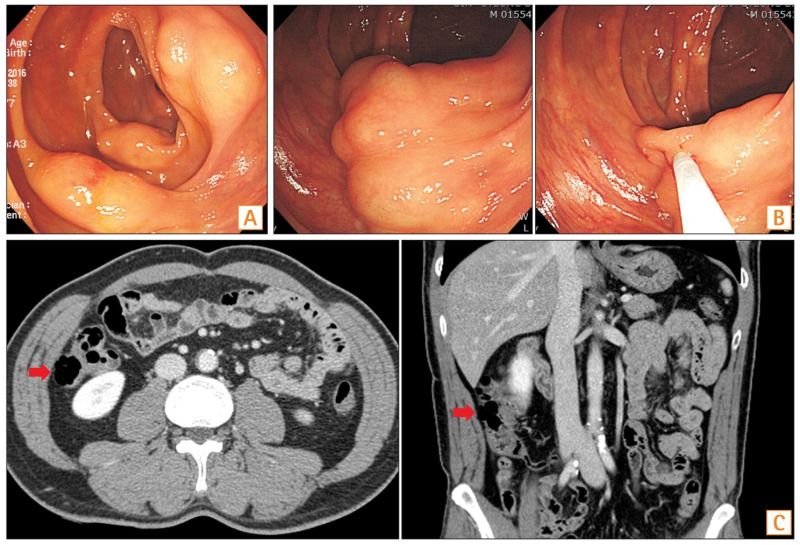
Question: A 54-year-old man visited Chungbuk National University Hospital outpatient clinic with abnormal colonoscopic findings at an outside hospital. He had been taking antihypertensive drugs and had undergone surgery for duodenal ulcer perforation approximately 30 years ago. He was a current smoker with no significant recent medical problems. There were no abnormalities noted on a colonoscopy 3 years ago, and he underwent a screening colonoscopy at this time. Colonoscopy at our hospital showed multiple, variable-sized, round elevated lesions, with a smooth surface, noted in the ascending colon. They closely resembled subepithelial lesions (Fig. A). When the injection needle punctured and aspirated the lesions, they collapsed without releasing any fluid (Fig. B). CT of the abdomen showed multiple intramural air-containing cystic lesions in the ascending colon (Fig. C, arrows). We decided upon a conservative approach with only follow-up, because the patient was asymptomatic with no abnormalities noted on physical examination and laboratory studies. Colonoscopy and CT scan were performed a year later, which showed no significant changes in the multiple cystic lesions seen in the ascending colon. The patient continued to be asymptomatic with no abnormalities noted on physical examination and laboratory studies. What is the diagnosis of the multiple cystic lesions in the colon?
Answer to the Images: Pneumatosis Intestinalis
Pneumatosis intestinalis (PI) is a rare condition representing the presence of gas in the bowel wall. PI is associated with numerous conditions, ranging from benign to life threatening ones.1 A number of synonyms for PI have been reported in literature, viz., pneumatosis cystoides intestinalis, intramural gas, pneumatosis coli, pseudo-lipomatosis, intestinal emphysema, bullous emphysema of the intestine, and lymphopneumatosis. PI can occur in any age group, ranging from neonates to elderly patients.2 The exact incidence of PI is unknown because most patients with PI are asymptomatic. An autopsy series reported an incidence of 0.03% in the general population.1
PI can occur anywhere within the gastrointestinal tract between the esophagus and the rectum but frequently occurs in the intestine. PI is idiopathic (15%) or secondary (85%) to a wide variety of gastrointestinal and non-gastrointestinal illnesses.3 Numerous hypotheses have been proposed to explain the pathogenesis of PI, including mechanical, bacterial, and biochemical causes. The cysts may be confined to the mucosa, submucosa, or subserosa, or involve all 3 layers. Most patients with PI are asymptomatic. When present, symptoms vary based on the location of PI, and include nausea, emesis, abdominal pain, diarrhea, abdominal distension, constipation, bloody stool, flatus, loss of appetite, weight loss, and tenesmus.2
PI may be discovered incidentally on screening sigmoidoscopy or colonoscopy. On gross appearance, submucosal cysts vary in size from a few millimeters to several centimeters and usually have a pale or bluish appearance, and when biopsied, can rapidly deflate with an audible hiss.4 Mucosal (e.g., adenomas and colitis cystica profunda) or submucosal lesions (e.g., lipoma and leiomyoma) can have an endoscopic appearance similar to PI. Assessment of patients with suspected PI should include a history evaluation, physical examination, laboratory studies, and abdominal imaging. On CT scan, PI usually appears as a low-density linear or bubbly pattern of gas in the bowel wall. There also may be circular collections of gas in the bowel wall.5 Decreased mural contrast-enhancement and the presence of associated portal venous gas are suggestive of intestinal ischemia.
Asymptomatic patients and those with mild symptoms can be managed as outpatients. Patients with moderate-to-severe symptoms require hospitalization. Treatment options include bowel rest, cessation of causative medications, antibiotics, octreotide, metoclopramide, erythromycin, high-flow oxygen, and hyperbaric oxygen therapy.2 Asymptomatic patients do not require additional therapy unless the patient becomes symptomatic. Intramural gas cysts usually resolve spontaneously over time.








