|
 |
- Search
| Intest Res > Volume 12(4); 2014 > Article |
|
Abstract
Background/Aims
Providers may be hesitant to perform double-balloon enteroscopy (DBE) in the elderly because the increased number of co-morbidities in this population poses a greater risk of complications resulting from sedation. There are limited data on the use of DBE in the elderly. Here, we assessed the safety and efficacy of DBE in the elderly compared to those in younger patients.
Methods
We retrospectively analyzed the medical records of 158 patients who underwent 218 DBEs. Patients were divided into an elderly group (age âĽ65 years; mean 71.4Âą5.4; n=34; 41 DBEs) and a younger group (age <65 years; mean 39.5Âą13.5; n=124; 177 DBEs).
Results
In both groups, the most common indication for DBE was obscure gastrointestinal bleeding. Mucosal lesions (33.3% vs. 60.9%; P=0.002) were the most common finding in both groups, followed by tumors (30.8% vs. 14.1%; P=0.036). The elderly were more likely to receive interventional therapy (51.3% vs. 23.5%; P=0.001). The diagnostic yield of DBE was slightly higher in the elderly group (92.3% vs. 86.5%; P=0.422), but was not statistically significant. The therapeutic success rate of DBE was 100% in the elderly group compared to 87.5% in the younger group (P=0.536). The overall DBE complication rate was 1.8% overall, and this rate did not differ significantly between the groups (2.6% vs. 1.7%; P=0.548).
Double-balloon enteroscopy (DBE) was introduced in 2003 in Korea and has been used in clinical practice for the past 10 years. DBE has become an important tool for the evaluation and management of small bowel diseases because it allows endoscopists to obtain biopsies of suspicious lesions, treat bleeding, and dilate small bowel strictures.1,2,3 According to previous studies, obscure gastrointestinal bleeding (OGIB) is the most common indication for DBE,4,5 and the diagnostic yield is 69.8-80.6%.6,7,8,9 The complication rate and therapeutic success rate are approximately 1-4% and 85-92%, respectively.5,7,10,11,12
The use of endoscopic techniques is increasing along with the continued increase of age-related diseases.13 The safety of conventional endoscopy and endoscopic retrograde cholangiopancreatography (ERCP) for elderly patients has been studied,14,15,16 and the results suggest these procedures are well tolerated in the elderly.
However, DBE-specific issues such as procedural complexity, complications, and extended procedure time may discourage certain providers from using DBE, especially in elderly patients who are at increased risk resulting from sedation owing to a higher incidence of co-morbidities. While a number of clinical studies on DBE have been published, there are little data on its use in elderly patients. In addition, most of these studies involved Western populations, and DBE outcomes have not yet been compared in young and elderly Korean patients. We therefore assessed the efficacy and safety of DBE in elderly patients compared to those in young patients.
This study was conducted at a tertiary care referral center. We retrospectively analyzed database records of all patients who had undergone DBE for small bowel evaluation between September 2003 and August 2013. A total of 158 patients and 218 DBE procedures were identified during the study period. Patients were divided into an elderly group (age âĽ65 years; n=34; 41 DBEs) and a younger group (age <65 years; n=124; 177 DBEs). Data collection and analysis were approved by the institutional review board of Soonchunhyang university hospital.
Endoscopy procedures for small bowel evaluation were performed with a commercially available DBE system (EN-450P5/20, T5/20; Fujinon Inc., Saitama, Japan). In DBE with an oral approach, the patient received nothing by mouth for at least 12 hours prior to the procedure. In DBE with an anal approach, patients were prepared similar to that for a colonoscopy with a 2 or 4 L polyethylene glycol-electrolyte lavage solution the day before the procedure. The approach was determined by the endoscopist based on the suspected location of target lesions, clinical judgment, capsule endoscopy (CE) findings, and/or radiologic imaging. All DBE procedures were performed under conscious sedation with midazolam and/or pethidine. Procedures were routinely performed with patients under monitored anesthesia care with a fluoroscopy unit. During the procedure, additional midazolam was administered selectively to achieve sufficient sedation. Patient status was determined by the American Society of Anesthesiologists (ASA) physical status classification system (Table 1).17 After DBE, all patients were monitored in the recovery room until fully recovered from sedation to observe the development of serious complications and manage them accordingly.
We analyzed DBE indications, positive findings, diagnostic yield, therapeutic success rate, and complications. Primary DBE indications were classified into seven categories based on previous studies: (1) OGIB; (2) abnormalities observed by another modality (e.g., CE or abdominal CT); (3) CD; (4) symptoms/signs only (e.g., abdominal pain, diarrhea, or weight loss); (5) therapeutic purposes (e.g., bleeding control, polypectomy, or removal of a foreign body); (6) surveillance (e.g., Peutz-Jeghers syndrome); and (7) others.3 Abnormalities observed using other modalities were suspected gastrointestinal lesions that required DBE for further confirmation. Positive findings were classified into five categories as follows: (1) vascular lesions (e.g., angioectasia, arterio-venous malformation, or varix); (2) mucosal lesions (e.g., CD, erythema, erosion, or ulcer); (3) tumor (benign or malignant); (4) others; and (5) no specific findings. These factors were compared between the elderly and younger groups.
Statistical analysis was performed using SPSS software, version 15.0 for Windows (SPSS Inc., Chicago, IL, USA). Continuous data are expressed as means and SDs. All continuous variables were compared using a two-tailed Student's t-test. All categorical variables were compared using Fisher's exact test. A P-value less than 0.05 was considered statistically significant.
Table 2 summarizes the baseline characteristics of the study patients. A total of 218 DBEs (n=158) were performed: 41 (n=34) in the elderly group and 177 (n=124) in the younger group. The mean age was 71.4 years (range, 65-88) in the elderly group and 39.5 years (range, 16-64) in the younger group. Co-morbidities were present in 67.6% of elderly patients and 33.9% of younger patients; the difference in the number of patients with co-morbidities between groups was statistically significant (P=0.001). The elderly group contained a significantly higher percentage of ASA class III patients (20.6% vs. 2.4%; P=0.001). A history of NSAID, anticoagulant, or antiplatelet agent use was significantly more common in the elderly group than in the younger group (29.4% vs. 11.3%; P=0.015). The most common imaging modality used prior to DBE was abdominal CT (66%) followed by CE (35%). Between-group differences in the use of previous imaging modality were not statistically significant.
In both groups, the most common indication for DBE was OGIB followed by abnormalities observed by other imaging modalities. The mean midazolam dose was 2.61 mg in the elderly group and 3.85 mg in the younger group, indicating a statistically significant difference (P<0.001). There was no difference in mean total procedure time between the elderly and younger groups (53.9Âą25.5 min vs. 58.6Âą28.6 min; P=0.347). Elapsed time to the deepest point was also not significantly different between the two groups. Table 3 summarizes procedure-related data according to group.
The overall DBE complication rate was 1.8% (4/218 DBEs). There were no significant differences in the complication rates between the elderly and younger groups (2.6% vs. 1.7%; P=0.548). One elderly patient (0.5%) was reported to have transient hypoxia during DBE, which alleviated with intraprocedural oxygen therapy. In the younger group, intervention-related bleeding (0.9%) was reported in two patients, and one patient was diagnosed with pancreatitis (0.5%) after DBE. All patients recovered with conservative treatment. No perforations or deaths related to DBE were reported (Table 3).
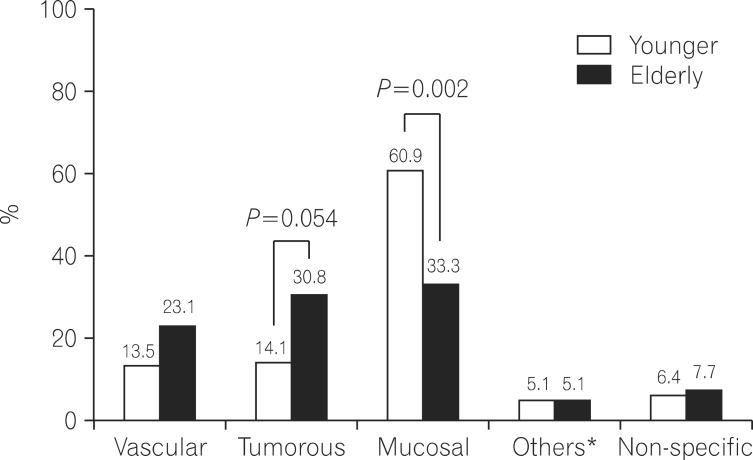
Figure 1 shows the final diagnoses of the study participants. The most common final diagnosis in both groups was mucosal lesion. Mucosal lesions were identified in a significantly higher percentage of younger patients, more than double the percentage of patients in the elderly group. In both groups, tumorous lesion was the second most common final diagnosis, occurring at a significantly higher frequency in the elderly group. Diagnostic yield was slightly higher in the elderly group than in the younger group, but this difference was not significant (92.3% vs. 86.5%; P=0.422). The concordance rate between DBE and CE findings was 70% in the elderly group and 51.6% in the younger group; the difference in the rate was also not significant.
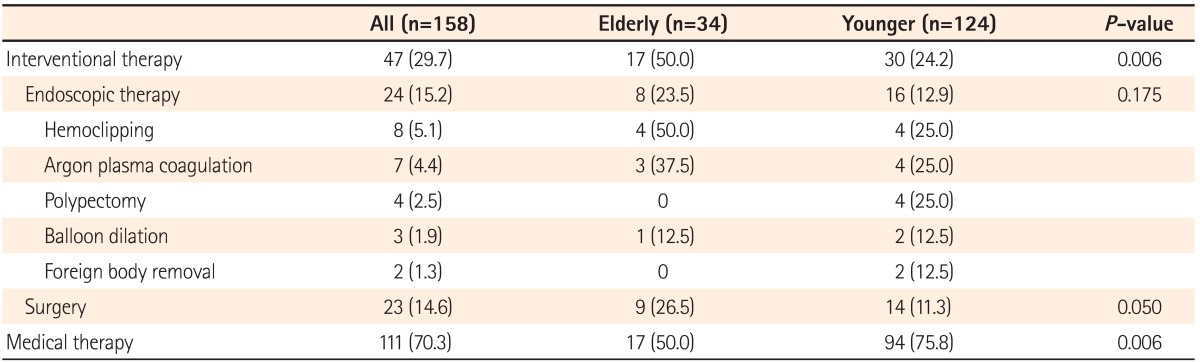
Interventional therapy (combined endoscopic therapy and surgery) was performed more frequently in the elderly group (50.0% vs. 24.2%; P=0.006). Hemoclipping was the most common endoscopic therapy, followed by argon plasma coagulation, polypectomy, balloon dilation, and foreign body removal. Medical therapy was administered to a higher percentage of younger patients than elderly patients (75.8% vs. 50.0%; P=0.006) (Table 4). The therapeutic success rate of DBE was 100% in the elderly group and 87.5% in the younger group, but the difference in the rate between groups was not statistically significant. Among patients who had undergone DBE for the diagnosis, therapeutic plans were determined in 45.7% (48/105) patients of the younger group and 51.6% patients of the elderly group (16/31) based on DBE results (P=0.683).
Currently, people worldwide can reach older ages because of advances in medical science. According to the latest demographic data18 released in 2013, the elderly comprise 12.2% of Korea's population, and this percentage is increasing. Based on data from 2011, the reported life expectancy of individuals aged 65 years and above was 17.4 years for men and 21.9 years for women.18 Because of this, the use of conventional endoscopy and ERCP in the elderly is rising, and the safety of these examinations has been confirmed.14,15,16 However, there are limited data on the safety and efficacy of DBE in the elderly, and no studies have compared DBE outcomes in the elderly and young Korean populations. We therefore assessed the efficacy and safety of DBE in the elderly compared to those in a younger age group and found that DBE is safe and effective in the elderly, providing a high diagnostic yield and high therapeutic success rate.
OGIB was the most common indication for DBE in both age groups in the present study. This was comparable to findings from a recent systematic review.3 In contrast to Western studies in which vascular lesions were the most common final diagnosis,3,6,9,19 mucosal lesions were most common in the present study, and there was a significantly higher percentage of mucosal lesions in the younger group. For mucosal lesions, the most common and detailed final diagnosis was drug-induced enteropathy in the elderly group and CD or tuberculosis in the younger group. In both age groups, the most common tumorous lesion was a gastrointestinal stromal tumor. This was similar to observations made in Eastern countries.8,20,21,22 According to previous studies, the diagnostic yield of DBE is around 60%.7,13,23 However, in the present study, though there was no significant difference between the age groups, the diagnostic yield in the elderly group was greater than 90%. It may have been elevated because, in some cases, DBE was performed on the basis of results obtained from previously used imaging modalities.
Interventional therapy combining endoscopic therapy and surgery was performed in a higher percentage of elderly than younger patients. Surgery was performed more frequently in the elderly group (26.5% vs. 11.3%; P=0.050) because significantly more tumorous lesions were found in that group. Previous studies reported that the therapeutic success rate of DBE was 72-92%.11,12 In the present study, the therapeutic success rate of DBE was also high in both age groups. In particular, endoscopic therapy with DBE was conducted successfully in 100% of the elderly group. This finding might be explained by the limited number of patients. We also suggest that endoscopists tend to perform intensive endoscopic therapy in elderly patients, in consideration of the age factor and underlying diseases. In addition, we found that therapeutic plans were determined in approximately half of the patients, showing the clinical importance of DBE in the elderly.
The overall complication rate in this study was 1.8%, similar to that observed in a previous study (1.2%).24 However, the 2.6% complication rate in the elderly group in the present study is lower than the 3.7% rate reported in a previous study that investigated the safety of DBE in 167 patients aged 75 years or older.9 This difference between the results of the present may be attributed to a difference in the age cut-off. In previous studies, age cut-offs of greater than 65, 70, 75, and 80 years were used to define "elderly" individuals.9,10,13,25 However, we used the traditional cut-off of 65 years used by the World Health Organization. It may be presumed that the inclusion of individuals aged 75 years and older in the previous study showed a higher complication rate in the elderly group. Interestingly, in another previous study with the same age cut-off (âĽ75 years), no major complications were observed in the elderly group, but complications such as transient hypoxia and transient cardiac arrhythmia occurred in patients younger than 75 years.10 A study from China in patients aged 65 years or older also found no severe DBE-related complications.13 Although complications one patient older than 65 years in the present study experienced complications, the patient's condition improved with conservative treatment. In this study, co-morbidities; ASA class III; and use of drugs such as NSAIDs, anticoagulants, or antiplatelet agents were present in a significantly higher percentage of elderly than younger patients. However, there were no statistically significant differences between the complication rates of the two groups. The mean midazolam dose was significantly lower in the elderly group than in the younger group (2.61 mg vs. 3.85 mg; P<0.001). A previous study suggested that the low complication rates in the elderly may be due to the modest doses of sedatives used in this population.24 If this theory is applied to the present study, it suggests that DBE safety can be improved by applying a more careful sedation procedure and closely monitoring elderly patients with co-morbidities.
We recognize the potential limitations of this study. First, it was a retrospective study, and we used data from a single center. Second, compared to previous studies, fewer high-risk elderly patients with an ASA classification of IV or greater were included in the present study. Therefore, selection bias may have occurred. Nevertheless, this is the first study to have compared DBE in elderly and younger Korean individuals, and to demonstrate that DBE is efficient and safe in the elderly.
In conclusion, although further evaluation based on larger, prospective, multi-center studies is needed to confirm our findings, DBE is safe and effective for elderly patients, and has a high diagnostic yield and high therapeutic success rate.
References
1. Yamamoto H, Sekine Y, Sato Y, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc 2001;53:216-220.PMID: 11174299.


2. Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc 2010;71:280-286.PMID: 20152309.


3. Xin L, Liao Z, Jiang YP, Li ZS. Indications, detectability, positive findings, total enteroscopy, and complications of diagnostic double-balloon endoscopy: a systematic review of data over the first decade of use. Gastrointest Endosc 2011;74:563-570.PMID: 21620401.


4. Raju GS, Gerson L, Das A, Lewis B. American Gastroenterological Association. American Gastroenterological Association (AGA) Institute technical review on obscure gastrointestinal bleeding. Gastroenterology 2007;133:1697-1717.PMID: 17983812.


5. Jeon SR, Kim JO, Kim HG, et al. Changes over time in indications, diagnostic yield, and clinical effects of double-balloon enteroscopy. Clin Gastroenterol Hepatol 2012;10:1152-1156.PMID: 22801056.


6. Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy 2006;38:42-48.PMID: 16429354.



7. Choi H, Choi KY, Eun CS, et al. Korean experience with double balloon endoscopy: Korean Association for the Study of Intestinal Diseases multi-center study. Gastrointest Endosc 2007;66:S22-S25.PMID: 17709024.


8. Zhong J, Ma T, Zhang C, et al. A retrospective study of the application on double-balloon enteroscopy in 378 patients with suspected small-bowel diseases. Endoscopy 2007;39:208-215.PMID: 17385105.



9. Byeon JS, Mann NK, Jamil LH, Lo SK. Double balloon enteroscopy can be safely done in elderly patients with significant co-morbidities. J Gastroenterol Hepatol 2012;27:1831-1836.PMID: 23034065.


10. Hegde SR, Iffrig K, Li T, et al. Double-balloon enteroscopy in the elderly: safety, findings, and diagnostic and therapeutic success. Gastrointest Endosc 2010;71:983-989.PMID: 20189563.


11. May A, Farber M, Aschmoneit I, et al. Prospective multicenter trial comparing push-and-pull enteroscopy with the single- and double-balloon techniques in patients with small-bowel disorders. Am J Gastroenterol 2010;105:575-581.PMID: 20051942.



12. Messer I, May A, Manner H, Ell C. Prospective, randomized, single-center trial comparing double-balloon enteroscopy and spiral enteroscopy in patients with suspected small-bowel disorders. Gastrointest Endosc 2013;77:241-249.PMID: 23043851.


13. He Q, Zhang Q, Li JD, et al. Double balloon enteroscopy in the old: experience from China. World J Gastroenterol 2012;18:2859-2866.PMID: 22719197.



14. Seinela L, Ahvenainen J, Ronneikko J, Haavisto M. Reasons for and outcome of upper gastrointestinal endoscopy in patients aged 85 years or more: retrospective study. BMJ 1998;317:575-580.PMID: 9721114.



15. Clarke GA, Jacobson BC, Hammett RJ, Carr-Locke DL. The indications, utilization and safety of gastrointestinal endoscopy in an extremely elderly patient cohort. Endoscopy 2001;33:580-584.PMID: 11473328.



16. Katsinelos P, Paroutoglou G, Kountouras J, Zavos C, Beltsis A, Tzovaras G. Efficacy and safety of therapeutic ERCP in patients 90 years of age and older. Gastrointest Endosc 2006;63:417-423.PMID: 16500389.


17. Asahq.org [homepage on the Internet]. IL: American Society of Anesthesiologists, Inc., c1995-2014:cited 2011 Apr 5. Available from: http://www.asahq.org/clinical/physicalstatus.htm.
18. Kostat.go.kr [homepage on the Internet]. Daejeon: Statistics Korea, Inc., c1996:cited 2013 Sep 30. Available from: http://sgis.kostat.go.kr/publicsmodel/#.
19. Seven G, Kozarek RA, Ross A, et al. Double balloon enteroscopy in a North American setting: a large single center 5-year experience. Intest Res 2013;11:34-40.

20. Nakamura M, Niwa Y, Ohmiya N, et al. Preliminary comparison of capsule endoscopy and double-balloon enteroscopy in patients with suspected small-bowel bleeding. Endoscopy 2006;38:59-66.PMID: 16429356.



21. Tanaka S, Mitsui K, Yamada Y, et al. Diagnostic yield of double-balloon endoscopy in patients with obscure GI bleeding. Gastrointest Endosc 2008;68:683-691.PMID: 18561920.


22. Sun B, Rajan E, Cheng S, et al. Diagnostic yield and therapeutic impact of double-balloon enteroscopy in a large cohort of patients with obscure gastrointestinal bleeding. Am J Gastroenterol 2006;101:2011-2015.PMID: 16848814.


23. Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB. Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. J Gastroenterol Hepatol 2011;26:796-801.PMID: 21155884.


24. Moschler O, May A, Muller MK, Ell C. German DBE Study Group. Complications in and performance of double-balloon enteroscopy (DBE): results from a large prospective DBE database in Germany. Endoscopy 2011;43:484-489.PMID: 21370220.



25. Qureshi WA, Zuckerman MJ, Adler DG, et al. ASGE guideline: modifications in endoscopic practice for the elderly. Gastrointest Endosc 2006;63:566-569.PMID: 16564853.


Fig. 1
Final diagnoses of study patients. In both groups, mucosal lesions were the most common finding, followed by tumorous lesions and vascular lesions. *Others represent Meckel's diverticulum and mucosal injury due to foreign body.
- TOOLS