|
 |
- Search
| Intest Res > Volume 20(3); 2022 > Article |
|
Abstract
Background/Aims
Methods
Results
ADDITIONAL INFORMATION
Funding Source
This work was supported by the Research Program, funded by the Korea Disease Control and Prevention Agency (2019-ER-6905-02).
Conflict of Interest
Kim YS is an editorial board member of the journal but was not involved in the peer reviewer selection, evaluation, or decision process of this article. No other potential conflicts of interest relevant to this article were reported.
Author Contribution
Conceptualization: Kim YS, Kim Seung Hyuk. Data curation: Kim YS, Kim Seung Hyuk. Formal analysis: Kim Seung Hyuk. Investigation: Kim YS, Kim Seung Hyuk, Lee SH, Lee HM. Methodology: Kim YS, Kim Seung Hyuk, Lee SH. Project administration: Kim YS. Resources: Kim YS, Kim Seung Hyuk. Software: Kim Seung Hyuk. Supervision: Kim YS. Validation: Kim Seung Hyuk, Moon JS. Visualization: Kim Seung Hyuk, Kim Seo Hyun, Myung HJ, Yoon WE. Writing - original draft: Kim YS, Kim Seung Hyuk. Writing - review & editing: Kim YS, Kim Seung Hyuk. Approval of final manuscript: all authors.
Fig.┬Ā1.
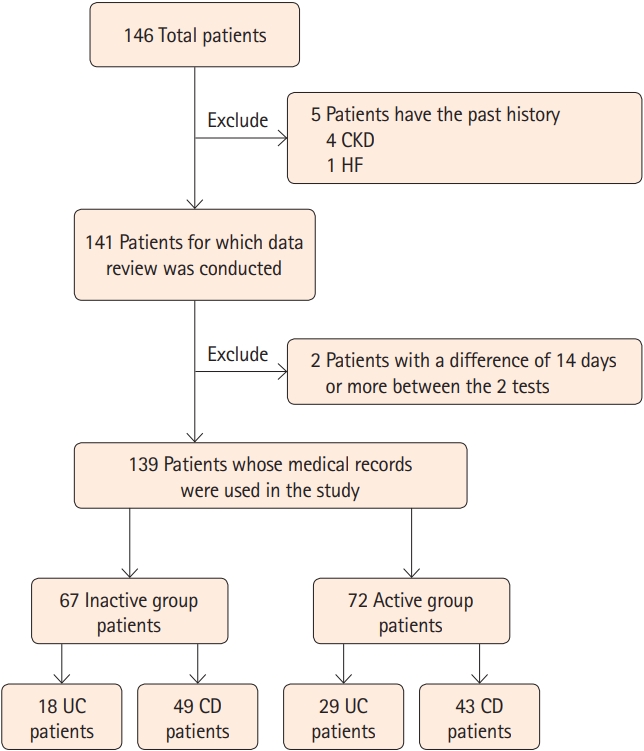
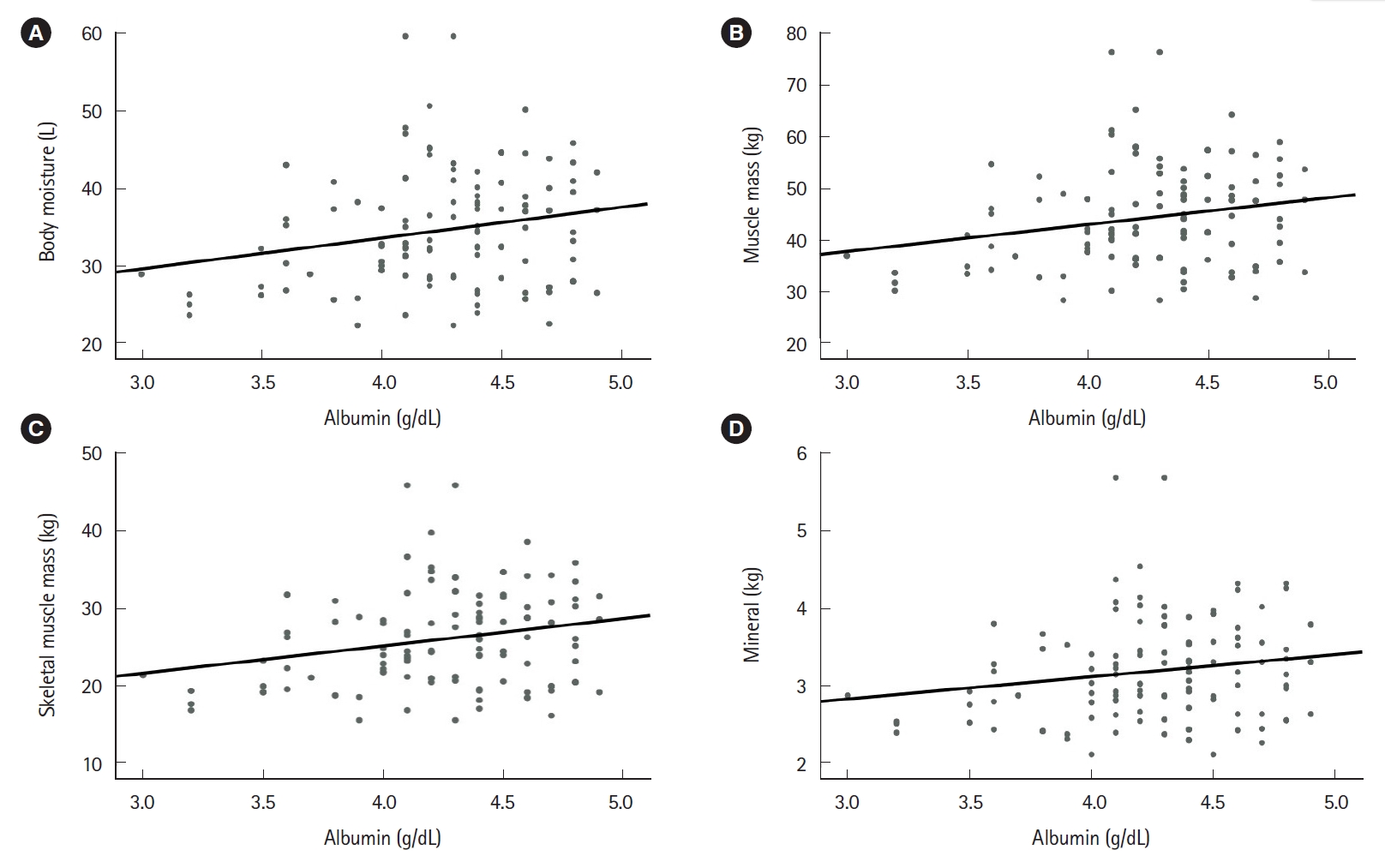
Fig.┬Ā2.
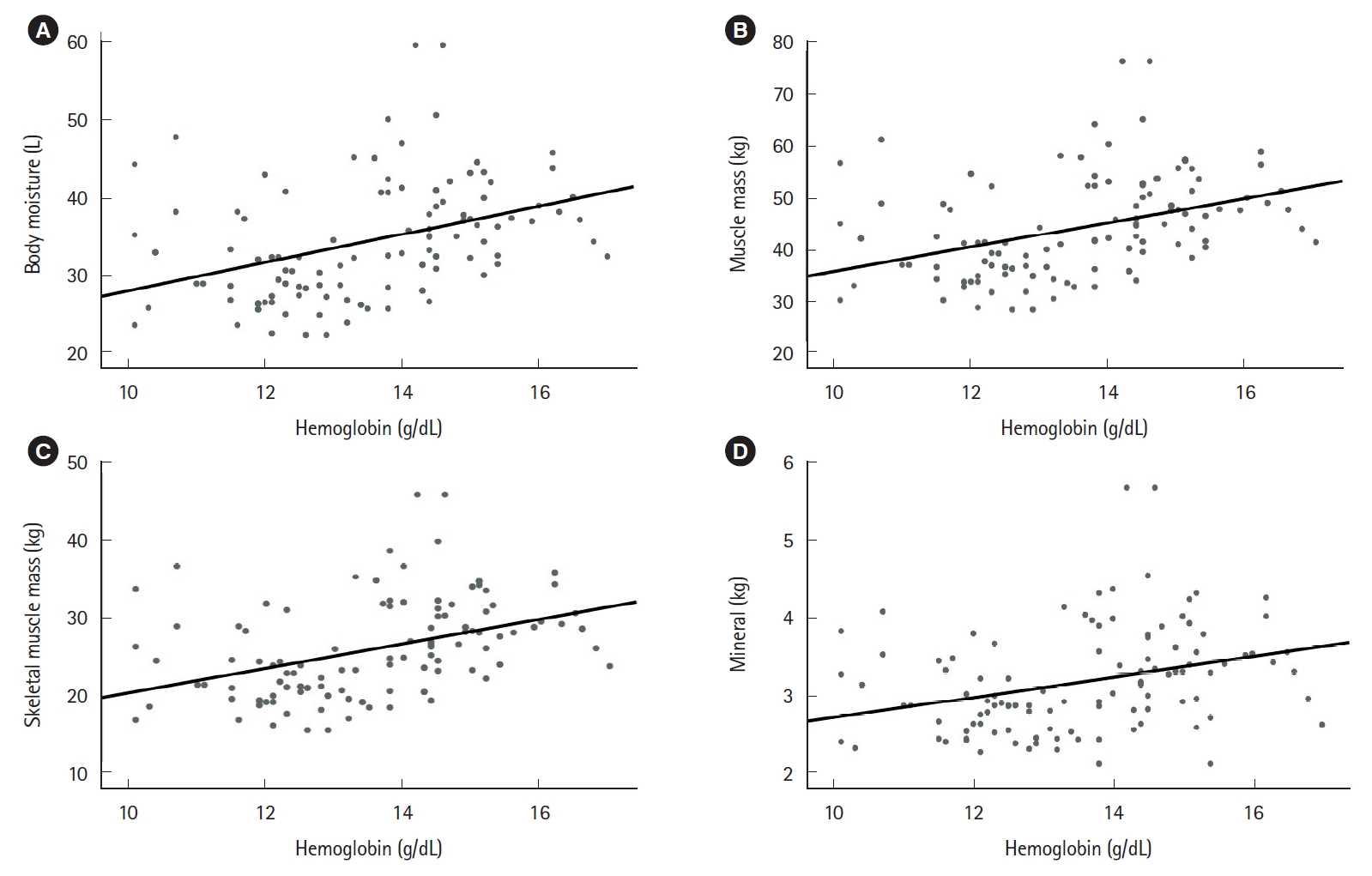
Fig.┬Ā3.

Fig.┬Ā4.
Table┬Ā1.
| Characteristic | Inactive (n = 67) | Active (n = 72) | P-valuea |
|---|---|---|---|
| Age (yr) | 48.55 ┬▒ 17.35 | 41.90 ┬▒ 17.56 | 0.026 |
| ŌĆāRange | 17-78 | 16-85 | |
| Sex | |||
| ŌĆāFemale | 22 (15.8) | 31 (22.3) | |
| ŌĆāMale | 45 (32.3) | 41 (29.5) | |
| Disease | |||
| ŌĆāUC | 18 (12.9) | 29 (20.9) | |
| ŌĆāCD | 49 (35.3) | 43 (30.9) | |
| Hemoglobin (g/dL) | 14.20 ┬▒ 1.48 | 13.07 ┬▒ 1.58 | < 0.001 |
| Total protein (g/dL) | 7.60 ┬▒ 0.44 | 7.18 ┬▒ 0.69 | < 0.001 |
| Albumin (g/L) | 4.46 ┬▒ 0.27 | 4.05 ┬▒ 0.44 | < 0.001 |
| Cholesterol (mg/dL) | 183.73 ┬▒ 33.80 | 172.38 ┬▒ 40.89 | 0.095 |
| Triglyceride (mg/dL) | 153.65 ┬▒ 135.49 | 129.56 ┬▒ 46.70 | 0.244 |
| ESR (mm/hr) | 17.73 ┬▒ 13.80 | 31.13 ┬▒ 20.45 | < 0.001 |
| CRP (mg/dL) | 0.26 ┬▒ 0.20b | 1.63 ┬▒ 2.91c | < 0.001 |
Table┬Ā2.
| Item | Inactive (n = 67) | Active (n = 72) | P-valuea |
|---|---|---|---|
| Body mass index (kg/m2) | 23.63 ┬▒ 3.82 | 22.23 ┬▒ 3.53 | 0.027 |
| Body moisture (L) | 35.69 ┬▒ 7.72 | 33.18 ┬▒ 7.72 | 0.047 |
| Muscle mass (kg) | 45.85 ┬▒ 9.98 | 42.60 ┬▒ 8.93 | 0.046 |
| Skeletal muscle mass (kg) | 26.90 ┬▒ 6.41 | 24.77 ┬▒ 5.74 | 0.042 |
| Mineral (kg) | 3.30 ┬▒ 0.69 | 3.07 ┬▒ 0.60 | 0.034 |
| Body fat (kg) | 17.26 ┬▒ 8.28 | 15.69 ┬▒ 6.34 | 0.212 |