|
 |
- Search
Article category
- Page Path
-
- HOME
- ARTICLE CATEGORY
- Article category
- IBD
- Colonic oncostatin M expression evaluated by immunohistochemistry and infliximab therapy outcome in corticosteroid-refractory acute severe ulcerative colitis
- Jim O’Connell, Jayne Doherty, Amy Buckley, David Cormican, Cara Dunne, Karen Hartery, John Larkin, Finbar MacCarthy, Paul McCormick, Susan McKiernan, Brian Mehigan, Cian Muldoon, Ciara Ryan, Jacintha O’Sullivan, David Kevans
- Intest Res. 2022;20(3):381-385. Published online March 11, 2022
- Full text PubReader ePub PDF Supplementary Material

- Microbiota
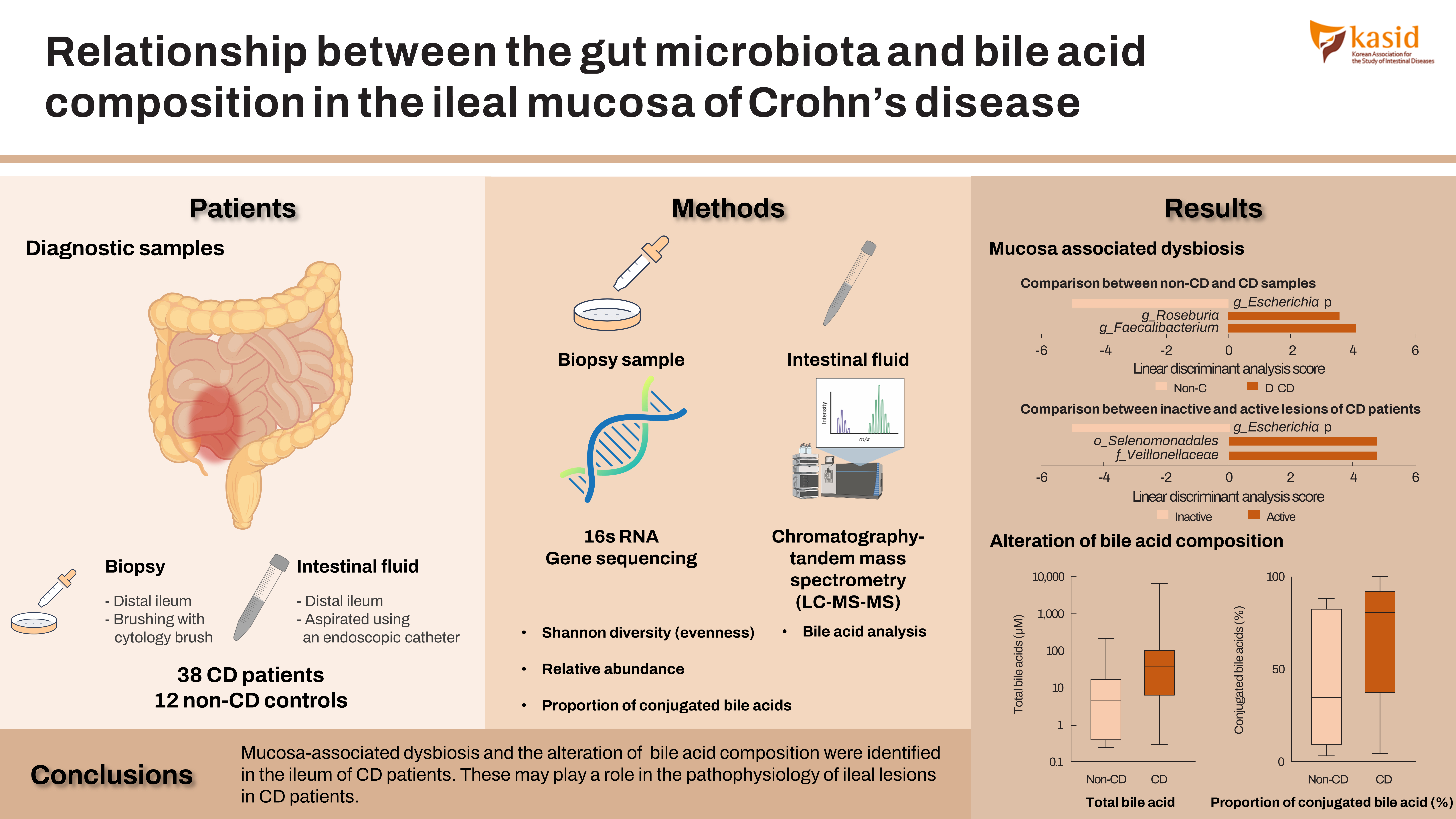
- Relationship between the gut microbiota and bile acid composition in the ileal mucosa of Crohn’s disease
- Shigeki Bamba, Osamu Inatomi, Atsushi Nishida, Masashi Ohno, Takayuki Imai, Kenichiro Takahashi, Yuji Naito, Junichi Iwamoto, Akira Honda, Naohiro Inohara, Akira Andoh
- Intest Res. 2022;20(3):370-380. Published online May 14, 2021
- Full text PubReader ePub PDF Supplementary Material

 |
 |
- IBD
- Intestinal ultrasonography and fecal calprotectin for monitoring inflammation of ileal Crohn’s disease: two complementary tests
- José María Paredes, Tomás Ripollés, Ángela Algarra, Rafael Diaz, Nadia Moreno, Patricia Latorre, María Jesús Martínez, Pilar Llopis, Antonio López, Eduardo Moreno-Osset
- Intest Res. 2022;20(3):361-369. Published online March 15, 2022
- Full text PubReader ePub PDF

 |
 |
- Clinical outcomes and predictors of response for adalimumab in patients with moderately to severely active ulcerative colitis: a KASID prospective multicenter cohort study
- Seung Yong Shin, Soo Jung Park, Young Kim, Jong Pil Im, Hyo Jong Kim, Kang-Moon Lee, Ji Won Kim, Sung-Ae Jung, Jun Lee, Sang-Bum Kang, Sung Jae Shin, Eun Sun Kim, You Sun Kim, Tae Oh Kim, Hyun-Soo Kim, Dong Il Park, Hyung Kil Kim, Eun Soo Kim, Young-Ho Kim, Do Hyun Kim, Dennis Teng, Jong-Hwa Kim, Wonyong Kim, Chang Hwan Choi, on behalf of the IBD Research Group of the Korean Association for the Study of Intestinal Diseases
- Intest Res. 2022;20(3):350-360. Published online July 23, 2021
- Full text PubReader ePub PDF Supplementary Material

 |
 |
- A nationwide analysis on the influence of obesity in inflammatory bowel disease hospitalizations
- Dushyant Singh Dahiya, Asim Kichloo, Farah Wani, Jagmeet Singh, Dhanshree Solanki, Hafeez Shaka
- Intest Res. 2022;20(3):342-349. Published online May 21, 2021
- Full text PubReader ePub PDF

 |
 |
- Real-world data for golimumab treatment in patients with ulcerative colitis in Japan: interim analysis in post-marketing surveillance
- Shiro Nakamura, Teita Asano, Hiroaki Tsuchiya, Kanami Sugimoto, Yuya Imai, Seiji Yokoyama, Yasuo Suzuki
- Intest Res. 2022;20(3):329-341. Published online August 4, 2021
- Full text PubReader ePub PDF Supplementary Material

 |
 |
- Evaluation of nutritional status using bioelectrical impedance analysis in patients with inflammatory bowel disease
- Seung Hyuk Kim, You Sun Kim, Si Hyeong Lee, Hyun Mi Lee, Won Eui Yoon, Seo Hyun Kim, Hee Jun Myung, Jeong Seop Moon
- Intest Res. 2022;20(3):321-328. Published online July 20, 2021
- Full text PubReader ePub PDF

 |
 |
- Risk factors for non-reaching of ileal pouch to the anus in laparoscopic restorative proctocolectomy with handsewn anastomosis for ulcerative colitis
- Shigenobu Emoto, Keisuke Hata, Hiroaki Nozawa, Kazushige Kawai, Toshiaki Tanaka, Takeshi Nishikawa, Yasutaka Shuno, Kazuhito Sasaki, Manabu Kaneko, Koji Murono, Yuuki Iida, Hiroaki Ishii, Yuichiro Yokoyama, Hiroyuki Anzai, Hirofumi Sonoda, Soichiro Ishihara
- Intest Res. 2022;20(3):313-320. Published online March 12, 2021
- Full text PubReader ePub PDF

 |
 |
- Factors associated with anti-tumor necrosis factor effectiveness to prevent postoperative recurrence in Crohn’s disease
- Anthony Buisson, Lisa Cannon, Konstantin Umanskiy, Roger D. Hurst, Neil H. Hyman, Atsushi Sakuraba, Joel Pekow, Sushila Dalal, Russell D. Cohen, Bruno Pereira, David T. Rubin
- Intest Res. 2022;20(3):303-312. Published online August 4, 2021
- Full text PubReader ePub PDF Supplementary Material

 |
 |
- Endoscopy for assessment of mucosal healing in ulcerative colitis: time bound or response guided?
- Ajit Sood, Ramit Mahajan, Arshdeep Singh, Vandana Midha, Varun Mehta
- Intest Res. 2022;20(3):297-302. Published online February 8, 2022
- Full text PubReader ePub PDF

 |
 |
- Landscape of inflammatory bowel disease in Singapore
- Daren Low, Nidhi Swarup, Toshiyuki Okada, Emiko Mizoguchi
- Intest Res. 2022;20(3):291-296. Published online January 7, 2022
- Full text PubReader ePub PDF

 |
 |
- Cancer
- Endoscopic diagnosis and treatment of early colorectal cancer
- Seung Wook Hong, Jeong-Sik Byeon
- Intest Res. 2022;20(3):281-290. Published online July 26, 2022
- Full text PubReader ePub PDF

 |
 |
- IBD
- Prevention of postoperative recurrence in Crohn’s disease: the never-ending story
- Jung-Bin Park, Sang Hyoung Park
- Intest Res. 2022;20(3):279-280. Published online July 26, 2022
- Full text PubReader ePub PDF

 |
 |
- Miscellaneous
- Endoscopic balloon dilations for strictures of rectum, ileocecal valve and duodenum in a patient with X-linked inhibitor of apoptosis deficiency: a case report
- Shinsuke Otagiri, Takehiko Katsurada, Kensuke Sakurai, Junichi Sugita, Naoya Sakamoto
- Intest Res. 2022;20(2):274-277. Published online February 8, 2022
- Full text PubReader ePub PDF

 |
 |
- IBD
- Correlation of fecal calprotectin and patient-reported outcome measures in patients with ulcerative colitis
- Nagesh Kamat, Sudheer K Vuyyuru, Saurabh Kedia, Pabitra Sahu, Bhaskar Kante, Peeyush Kumar, Mukesh Kumar Ranjan, Mukesh Kumar Singh, Sambuddha Kumar, Vikas Sachdev, Govind Makharia, Vineet Ahuja
- Intest Res. 2022;20(2):269-273. Published online February 8, 2022
- Full text PubReader ePub PDF Supplementary Material

 |
 |